Liver cirrhosis grading Child-Pugh class B: a Goliath to challenge in laparoscopic liver resection?—prior experience and matched comparisons
Introduction
Laparoscopic hepatectomy (LH) was fast developing in this decade, and at present, this new maneuver proved to be safe and effective in more and more minimal invasive surgical centers. In 2009, the first world congress of LH was held in Louisville, United States, and at that time, over 2,800 cases of LH for miscellaneous liver diseases were summarized (1). But, at that time, most of these LH cases reported were carried out in the form of “simple” liver resection, such as subcapsular resection, left lateral lobe resection and etc. Major hepatectomy were very rarely reported and only selectively performed in several high-volume center (2,3). However, in 2014, during the 2nd International Consensus Conference on LH in Iwate, Japan (4), lots of challenging and new techniques and theories were witnessed. Nowadays, LH could be utilized in the donors of liver transplantation (5,6), and there were already some reports on left or right hemihepatectomy (3), and even in spiegel caudate lobe (segment I) (7). Probably, the concept of “laparoscopic segments”, which meant segment II, III, IVa, V, VI was already out-dated, and should be refined.
Bleeding control is the eternal topic in LH. Intra-operative bleeding would be much more difficult in the background of liver cirrhosis, and immense bleeding would increase the risk of post-operative liver failure. In cirrhotic cases grading Child-Pugh class A, there were already some experiences to successfully manipulate LH (8-13) (Table 1). However, whether LH could be safely performed in Child-Pugh class B and C patients were very rarely studied.
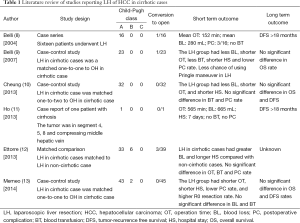
Full table
Sir Run Run Shaw Hospital in Zhejiang, China is one of a high-volume LH centers in Asia. Our first case of LH was successfully performed in 1998, and in the year of 2014, we published our experience for over 350 cases (14). At the same time, we built our own databases for all our LH cases. In this study, we reviewed this database for patients grading Child-Pugh class B/C. Furthermore, we compared these Child B/C cases to Child A cases undergoing LH for peri-operative information.
Methods
Patients
This study was of retrospective nature. Its design was approved by the Ethnic Committee of Sir Run Run Shaw Hospital affiliated with Zhejiang University, China. All cases in the LH database were carefully checked. At last, over 30 patients with liver cirrhosis were identified. Their medical documents were carefully reviewed, and their Child-Pugh scores were graded. The utilization of Child-Pugh system was strictly followed with the system proposed by Pugh Rn in 1973, that is, the score was based on encephalopathy (1, none; 2, minimal; 3, coma), ascites (1, absent; 2, controlled; 3, refractory), billirubin (1, <34 µmol/L; 2, 34-51 µmol/L; 3, >51 µmol/L), albumin (ALB) (1, >35 g/L; 2, 28-35 g/L; 3, <28 g/L), prothrombin (1, <4 s; 2, 4-6 s; 3, >6 s) (15). Based on computation, five patients were graded as Child-Pugh class B (7-9 points), and the left cases were graded as Child-Pugh class A (5-6 points). No case was graded as Child-Pugh class C (over 10 points).
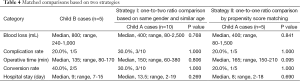
To compare Child B cases with Child A cases undergoing LH, we used two strategies for comparisons. The first one was a one-to-two ratio comparison based on same gender and similar age (difference was within ten years). However, this strategy had intrinsic deficiencies for confounding covariates such as the location of lesion, size of tumor, year for operation and etc. Therefore, we also manipulated the second form of matching strategy: propensity score matching. In this strategy, propensity score of each Child B or A patient was calculated based on a binary logistic regression considering five covariates as the year for operation, gender, infection with hepatitis B, maximum diameter of tumor and location of tumor (segment I-IV or segment V to VIII). After that, Child B cases were matched to Child A cases with a one-to-one ratio manner based on the principle of nearest neighbor matching (similar statistical teaching video with SPSS was available in “Ayumi’s Biostats Lesson” at https://www.youtube.com/watch?v=u-Kw1CAxjuI). Between Child B and Child A cases, peri-operative information including blood loss (BL), complication rate, operative time, conversion rate and hospital stay (HS) were compared.
Surgical maneuver
Our surgical maneuvers were described in previous literatures (16,17). High-quality enhanced CT scanning of the upper abdominal part was necessary in all cases. In selected cases, enhanced magnetic resonance (MR) and indocyanine green (ICG) retention test were considered. Generally, we used a five-hole strategy to place trocars on the abdomen of patients. A surgical team to perform LH consisted of three surgeons, as the chief surgeon to manipulate, first assistant for retraction and the second assistant to control the air flow for aspiration of. laparoscopic Peng’s multifunctional operative dissector (LPMOD).
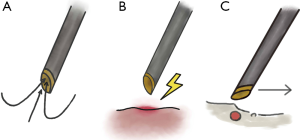
Nowadays, several powerful instruments are frequently used in LH, including ultrasonic dissector, cavitron ultrasonic surgical aspirator (CUSA), Ligasure, linear stapler and Habib 4X devices. Unlike other high-volume centers, we developed a very unique instrument as LPMOD (Figure 1). LPMOD was developed on the basis of the Peng’s multifunctional operative dissector (PMOD) for open hepatectomy (18). According to our experience, the merits of LPMOD were as follows: (I) multifunction. LPMOD could be used for aspiration, electronic coagulation, blunt dissection of vessels and liver parenchyma, which previously must be executed by different instruments. Therefore, the time cost by shifting different instruments could be saved, and the surgical team would be more focused on their meticulous manipulations (Figure 2); (II) utilization of a novel skill named “Curettage and Aspiration” technique (19,20). It means during transection, the liver parenchyma was crashed and aspirated immediately, and intra-hepatic ducts and small vessels could be safely identified. This technique was impossible to be carried out by ultrasonic dissector, Ligasure, linear stapler or Habib, probably achievable by CUSA in open hepatectomy (with help from skilled first assistance). But, only by LPMOD, “Curettage and Aspiration” technique was possible to be handled by one surgeon.

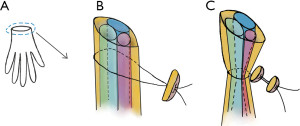
Other surgical instruments we generally used during LH were as follows: (I) laparoscopic ultrasound to locate the place of tumor; (II) grasping forceps to draw the liver capsule for retraction, sometimes the fan-retractor; (III) curved dissecting forceps to mobilize vessels and ducts, and in some cases we would use 90-degree curved forceps; (IV) “Pringle maneuver instrument” to control bleeding. The instrument consisted of one rim of a glove and two hem-o-locks (Figure 3); (V) titanic clips to clamp small vessels with their diameters less than 1 mm; (VI) absorbable clips and non-absorbable polymer clips to close bigger vessels; (VII) linear stapler to close major hepatic veins (right, left and etc.); (VIII) needle holding forceps to suture in some cases. In every case, a drainage tube would be placed near the cutting surface. When the fluid is less than 30 mL every day, and no evidence of bile leakage or abdominal infection exist, the tube would be drawn.
Statistical analysis
The data were statistically analyzed using the SPSS statistical software packages, version 16 (SPSS, Inc., Chicago, IL, USA). The continuous variables were compared by using the Mann-Whitney test. The categorical variables were compared by using the Pearson’s χ2 test or Fisher’s exact test depending on sample size. P<0.05 was considered statistically significant.
Results
Five patients grading Child B were included in this study. All of them were male, and during pathological examination, their diseases were confirmed as hepatocellular carcinoma (HCC). Their basic characteristics and the reasons for their Child-Pugh grading were listed in Table 2. The median age was 60 (range, 27-79) years, four in five patients were infected with HBV, three patients were grades as 7 points and 2 patients were graded as 8 points. None of the patients in our study presented with encephalopathy.
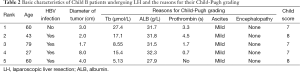
Full table
The peri-operative outcome of each patient was summarized in Table 3. All of the patients underwent non-anatomical liver resection. Among them, two of them were converted to open due to incidental finding of multiple hepatic metastasis (case No. 4), and difficulty for exposure and manipulation (case No. 5). The median BL was 800 (range, 240-1,000) mL, median operative time was 135 (range, 80-170) min, and median length of HS was 9 (range, 7-15) days. There was no post-operative mortality. Post-operative complication happened in one patient (case No. 3, pulmonary infection).

Full table
Matched comparison was conducted with two strategies. The first one was a one-to-two ratio comparison based on same gender and similar age. No statistical difference was observed for BL, complication rate, operative time, open rate and HS (P>0.05). Similar conclusion was achieved with a one-to-one ratio propensity score matching (Table 4).
Full table
Discussion
Except for its cosmetic merit, the advantages of LH are as follows: less surgical injury, faster recovery, lower complication rate and etc. (21,22). Based on the concept of “fast track surgery”, the idea of performing LH in the background of chronic liver diseases would be very attractive. Although high-volume evidence or RCT were lacking on LH in cirrhotic liver, two conclusions could possibly be drawn from current literatures (Table 1): (I) in selected cases, LH in cirrhotic cases had the potential to be better than OH; (II) in Child A patients, LH proved to be safe and feasible. However, very few cases were attempted in liver cirrhosis grading Child B/C [only 6 Child B cases in the study of Ettorre et al. (12) and 2 Child B cases in the study of Memeo et al. (13), no Child C cases]. In severe cirrhotic cases, the most challenging technical point is bleeding control. Two much BL is not only the reason for conversion to laparotomy, but also for postoperative insufficiency of liver function. Although miscellaneous powerful instruments were introduced into LH, including CUSA and ultrasonic dissector, none of them are ideal to control immense BL intra-operatively. Based on our surgical experience, LPMOD seemed to be much more efficient in hemostasis compared with other instruments, especially when the surgeon manipulates “Curettage and Aspiration” technique proficiently.
But, the utilization of an excellent instrument does not automatically guarantee success. A long progress to master correlative technique, or “learning curve”, is necessary for LH in the background of severe cirrhosis or chronic liver diseases. Until now, there were no reports of learning curve in cirrhotic cases. Anyway, in our opinion, a surgeon qualified to do LH with cirrhosis should be a master in all types of LH, otherwise he or she should not challenge such difficult situations. In our center, we had summarized “learning points” of different types of LH (14). For left lateral hepatectomy, the learning point was 43 cases, and for non-anatomic liver resection (mainly wedge resection), the learning point was 35 cases. Major hepatic resection would be much more difficult, and for left hemihepatectomy, the learning point should be among 15-30 cases, and for right hemihepatectomy, the cases would possibly be more. Without adequate skill in major hepatic resection, we did not suggest attempts in cirrhotic case.
Our study is the first to prove that in Child-Pugh class B, LH might be as safe as in Child-Pugh class A patients. The major limitation of our study was small volume of patients, which is due to the extreme difficulty to perform this procedure. However, by two ways of matched comparison (comparison based on same sex and similar age, and propensity score matching), BL, complication rate, operative time, conversion rate and HS were proved to be as good as in Child B patients compared with Child A patients. This conclusion proved that for experienced specialists of LH, LH in selected Child-Pugh class B patients should not be considered as a contradiction but to be worthy of attempts, just as a Goliath to face and fight.
This study did not answer whether LH could be safely performed in patients with Child C. Surely, Child C patients need to be more carefully evaluated with multiple preoperative examinations. And the decision would better to be made in a multidisciplinary team (MDT) manner, including the department of surgery, radiology, hepatology, and intensive care unit if necessary. Also, master-level surgical skill would be necessary.
Conclusions
In conclusion, selected Child B patients could be attempted to receive LH, and the postoperative effect would probably be as good as Child A patients. Whether LH could be safely performed in patients grading Child C needs further exploration.
Acknowledgements
Funding: This study was supported by the Fundamental Research Funds for the Central Universities (2014FZA7005).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Ethnic Committee of Sir Run Run Shaw Hospital affiliated with Zhejiang University, China.
References
- Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg 2009;250:831-41. [PubMed]
- Dagher I, O’Rourke N, Geller DA, et al. Laparoscopic major hepatectomy: an evolution in standard of care. Ann Surg 2009;250:856-60. [PubMed]
- Lin NC, Nitta H, Wakabayashi G. Laparoscopic major hepatectomy: a systematic literature review and comparison of 3 techniques. Ann Surg 2013;257:205-13. [PubMed]
- Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 2015;261:619-29. [PubMed]
- Cherqui D, Soubrane O, Husson E, et al. Laparoscopic living donor hepatectomy for liver transplantation in children. Lancet 2002;359:392-6. [PubMed]
- Laurent A, Tayar C, Andréoletti M, et al. Laparoscopic liver resection facilitates salvage liver transplantation for hepatocellular carcinoma. J Hepatobiliary Pancreat Surg 2009;16:310-4. [PubMed]
- Cai XJ, Dai Y, Yu H, et al. A case report of retrograde laparoscopic Spiegel lobectomy: an alternative surgical procedure. Chin Med J (Engl) 2009;122:596-8. [PubMed]
- Belli G, Fantini C, D’Agostino A, et al. Laparoscopic liver resections for hepatocellular carcinoma (HCC) in cirrhotic patients. HPB (Oxford) 2004;6:236-46. [PubMed]
- Belli G, Fantini C, D’Agostino A, et al. Laparoscopic versus open liver resection for hepatocellular carcinoma in patients with histologically proven cirrhosis: short- and middle-term results. Surg Endosc 2007;21:2004-11. [PubMed]
- Cheung TT, Poon RT, Yuen WK, et al. Long-term survival analysis of pure laparoscopic versus open hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a single-center experience. Ann Surg 2013;257:506-11. [PubMed]
- Ho CM, Wakabayashi G, Nitta H, et al. Total laparoscopic limited anatomical resection for centrally located hepatocellular carcinoma in cirrhotic liver. Surg Endosc 2013;27:1820-5. [PubMed]
- Ettorre GM, Laurenzi A, Lionetti R, et al. L aroscopic liver resections in normal and cirrhotic livers: a retrospective analysis in a tertiary hepato-biliary unit. Dig Liver Dis 2014;46:353-7. [PubMed]
- Memeo R, de’Angelis N, Compagnon P, et al. Laparoscopic vs. open liver resection for hepatocellular carcinoma of cirrhotic liver: a case-control study. World J Surg 2014;38:2919-26. [PubMed]
- Cai X, Li Z, Zhang Y, et al. Laparoscopic liver resection and the learning curve: a 14-year, single-center experience. Surg Endosc 2014;28:1334-41. [PubMed]
- Durand F, Valla D. Assessment of the prognosis of cirrhosis: Child-Pugh versus MELD. J Hepatol 2005;42 Suppl:S100-7. [PubMed]
- Cai XJ, Yang J, Yu H, et al. Clinical study of laparoscopic versus open hepatectomy for malignant liver tumors. Surg Endosc 2008;22:2350-6. [PubMed]
- Cai XJ, Wang YF, Liang YL, et al. Laparoscopic left hemihepatectomy: a safety and feasibility study of 19 cases. Surg Endosc 2009;23:2556-62. [PubMed]
- Peng SY, Li JT. “Curettage and aspiration dissection technique” using PMOD for liver resection. HPB (Oxford) 2008;10:285-8. [PubMed]
- Cai XJ, Yu H, Liang X, et al. Laparoscopic hepatectomy by curettage and aspiration. Experiences of 62 cases. Surg Endosc 2006;20:1531-5. [PubMed]
- Cai XJ, Liang X, Wang YF, et al. Laparoscopic hepatectomy by curettage and aspiration: a new technique. Chin Med J (Engl) 2007;120:1773-6. [PubMed]
- Viganò L, Tayar C, Laurent A, et al. Laparoscopic liver resection: a systematic review. J Hepatobiliary Pancreat Surg 2009;16:410-21. [PubMed]
- Simillis C, Constantinides VA, Tekkis PP, et al. Laparoscopic versus open hepatic resections for benign and malignant neoplasms--a meta-analysis. Surgery 2007;141:203-11. [PubMed]


