Living donor liver transplantation in Taiwan—challenges beyond surgery
Introduction
Living donor liver transplantation (LDLT) is a complex endeavor and a vast array of human resources, technology and infrastructure require to be harnessed for establishing a successful liver transplant program. Taiwan was a relatively small developing country at the time of inception of LT, but presently LDLT in Taiwan is among the best in the world when measured in terms of survival outcomes, scientific research or patient volumes per million population (1,2). The course of development of LDLT in Taiwan may have some illuminating lessons, especially with reference to the prospects of liver transplant programs in many countries which are making the transition from low-income to middle and even high-income nations.
Starzl attempted the first human liver transplant in 1963 (3). The survival and complication rates over the next couple of decades were daunting, pointing to the tremendous technical challenges associated with the procedure, in addition to the immunologic challenges. Consequently, continuous innovations in surgery and immunosuppression, particularly the development of cyclosporine, gave a boost to the field.
Taiwan had a relatively high incidence of end-stage liver disease and hepatocellular carcinoma (HCC). Like other countries in East Asia, Taiwan had among the highest incidence of hepatitis B virus (HBV) carriers in the world (4). The incidence of hepatitis C virus (HCV) infection in the population was also relatively high, especially in some regions and communities (5-7). The high incidence of viral hepatitis has translated to a high burden of cirrhosis, end-stage liver failure and HCC (8). The healthcare challenges involved in managing chronic liver disease in Taiwan were quite formidable.
Initial challenges in transplantation
The East Asian tiger economies including Taiwan began prospering economically in the last quarter of the twentieth century. Local healthcare groups and the government invested in improving and expanding hospital resources, establishing laboratories, personnel training, etc., and provided the means for providing better healthcare. Health services improved significantly. The high incidence of liver diseases led to the local doctors becoming expert at surgical treatment of liver tumors. However, at that time LT was attempted only at select centers, mainly in the United States and Europe. Despite difficulties such as diplomatic issues and language barriers, talented doctors from Taiwan studied at centers of excellence in the United States, Japan and other advanced countries. A conjunction of all these factors helped Taiwan over the next few decades.
The first successful deceased donor liver transplant (DDLT) in Taiwan was done at Chang Gung Memorial Hospital in 1984 for Wilson’s disease (9). The concept of brain death was used and documented thoroughly. The vigorous public discussion resulting from the transplant, along with the awareness of the need for such procedures and evidence of successful outcome helped in accepting liver transplant as a life-saving procedure. Consequently, Taiwan became the first in Asia to frame legislation for organ donation. The use of cyclosporine aided in achieving acceptable immunosuppression after transplantation. Split liver transplants were also performed and grafts were even shared across national borders, demonstrating that saving lives is the paramount aim in medicine (10).
Despite the excellent outcomes, the concept of brain death and organ donation was far less acceptable in East Asian countries compared to the West. The prevailing cultural values attached enormous importance to families and ancestors. The attitude that cadaveric donation would desecrate the deceased person’s spirit, combined with dismal outcomes in certain countries, resulted in considerable reluctance to get involved with organ donation (1). In addition, the lack of pediatric cadaveric donors led to the development of split LT.
Development of LDLT in Taiwan
In contrast to the perception of DDLT, there was widespread acceptability of the idea of LDLT in East Asia. The ethical considerations in pediatric LDLT were reasonably clear and without suspicion of coercion. However, technical factors of the procedure and donor safety had to be thoroughly ensured. By this time, there was accumulation of technical expertise acquired over the years with liver resections and DDLT. There was extensive cooperation among Asian liver surgery centers. Coordinated animal experiments were conducted, between Japanese and Taiwanese doctors (11). All these efforts culminated in the first LDLT in Taiwan in 1994, with successful long term survival (12). Over time, some of the largest case series in the world for LDLT for biliary atresia, along with other metabolic liver diseases were reported from Taiwan (13,14).
The first adult LDLT in Taiwan was done in 1999. Over the next decade, the volumes of LDLT continued to rise in Taiwan, but at a far steeper rate than DDLT. The extensive interactions with other East Asian centers helped in exchange of ideas and information, regarding technical aspects of the surgery. Preoperative radiologic imaging also improved by leaps and bounds (15). Transplant anesthesia, pathology and gastroenterology also developed significantly (16). The donor hepatectomy procedure was refined (17) and left lobe LDLT introduced in suitable cases to further reduce donor morbidity. Chronic end stage liver disease due to viral hepatitis was the commonest indication for adult LDLT. Dual graft LDLT was performed for the first time in Taiwan in 2002 (18).
Advances in LDLT
Over time, various innovative techniques were developed or refined in Taiwan. In pediatric LDLT, reduced left lateral grafts and mono-segment grafts were used for small infants. Techniques were developed for obtaining a wide outflow tract in the graft (19). With proper anesthetic management, blood transfusion for recipients could be avoided (16). Perioperative portal vein stenting enabled establishment of proper portal flow in cases of biliary atresia with small, hypoplastic and sclerotic portal veins (20,21). Similarly, there was incremental improvement in techniques of adult LDLT over time. Assessment of fatty liver in the donor (22), as well as challenging cases due to hepatic anatomy, volumetry and ABO incompatibility (ABOi) were done. Dual grafts were utilized when graft volume of single donor was insufficient (18). Techniques for outflow reconstruction (23,24) including the venous drainage of the right anterior sector as well as management of extensive portal thrombosis in the recipient were improved. Technical challenges such as presence of extensive adhesions due to multiple previous procedures and retransplantations were refined continually (19). The hepatic arterial anastomosis and the biliary reconstruction were routinely done by an expert microsurgeon using the operating microscope, leading to low rates of arterial and biliary complications (25-28). The gastric arteries, particularly the right gastroepiploic artery were used as an alternate inflow source if the native hepatic arteries were unsuitable (29). Selective portal inflow modulation was practiced, enabling higher number of left lobe LDLT and hence increased donor safety, while avoiding small for size syndrome in the recipient. Immunosuppression protocols were refined over time, with calcineurin inhibitors (cyclosporine and tacrolimus) forming the mainstay, in addition to the introduction of mammalian Target of Rapamycin (mTOR) inhibitors such as sirolimus and everolimus for adult recipients at risk of HCC recurrence or having renal impairment. The introduction of basiliximab for induction of immunosuppression in adult recipients has had a renal sparing effect over the long term (30).
Recurrence of hepatitis B and hepatitis C, as well as de novo infections after transplantation are a significant problem in LT. Strategies for using pretransplant hepatitis B vaccination and/or posttransplant antiviral drugs for pediatric patients receiving hepatitis B core antibody (HBcAb) positive grafts were developed (31,32). The HBV recurrence rate after transplant has reduced to 1.37% after the routine use of low dose hepatitis B immunoglobulin and entecavir (32). The newly introduced direct-acting antiviral (DAA) drug regimens for hepatitis C have enabled achievement of high sustained virologic response before and after transplantation, and hence remarkably reduce the chances of recurrence. The guidelines mandated by the Taiwan National Health Insurance for accepting HCC patients for transplant were expanded in 2006 to the University of California, San Francisco (UCSF) criteria from the Milan criteria (33). Various studies from Taiwan showed that cases beyond the UCSF criteria could be downstaged by trans-arterial embolization, radiofrequency ablation or percutaneous ethanol injection; and the recurrence rates in these patients after transplantation were similar to those within the UCSF criteria, who did not require downstaging (34,35).
Present status of LDLT in Taiwan
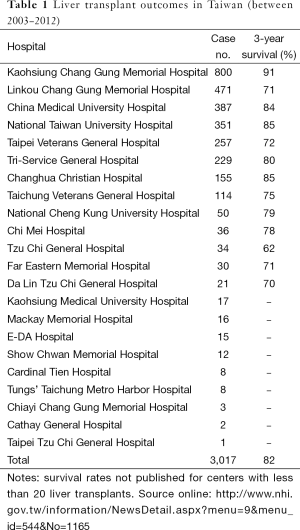
The presence of universal coverage by the Taiwan National Health Insurance enabled the establishment of clear guidelines for donor selection criteria, indications and timing for LT. They also regularly published the organ transplantation outcomes to ensure public awareness and transparency. There were 24 centers approved by the Ministry of Health and Welfare, which performed 3,017 liver transplants in Taiwan between 2003 and 2012, with an overall 3-year survival rate of 82% (Table 1). The highest volume center (Kaohsiung Chang Gung Memorial Hospital) also had the highest 3-year survival rate of 91% (36). The 1- and 5-year survival rates for pediatric LDLT for biliary atresia at this center (98% each) were among the highest in the world (13).
Full table
The way ahead
Increased volumes at the top centers have also increased the competence of associated departments like gastroenterology (for perioperative management) and radiology (perioperative imaging, interventional procedures) (37). Future development of LDLT in Taiwan shall not be purely a numbers game. The incidence of HCC has started to decline from 1995 and correlates strongly with the initiation of national immunization program for hepatitis B and the coverage of antiviral drugs and interferon in the national health insurance system (38). There has been a gradual but significant decrease in the incidence of HBV carriers. There has been an increase in the number of overseas patients seeking LDLT in Taiwan, and hospitals have established a framework for helping these patients (39). At the same time, there are numerous lessons for society and the healthcare system. The social and cultural milieu of the country, especially the close family bonds, as well as universal literacy, excellent primary care hospitals, good transport and ambulance facilities, a national health insurance system, competent social workers to interact and assess the families, electronic sharing of patient information securely between different treatment facilities, etc., have all helped in improving outcomes of the transplant procedure. The top transplant centers have also accumulated a wealth of experience, and established good protocols for patient management and quality of care. They have been actively pursuing translational research for further elucidation of the molecular basis of liver diseases. On the clinical front, promising developments in LDLT include the development of newer and more affordable drugs for hepatitis C and minimally invasive donor hepatectomy, while other advances such as increased use of smaller grafts without development of small for size syndrome, development of ABOi transplantation and expanded criteria for HCC still need to be further refined before widespread acceptance.
Conclusions
LT in Taiwan developed with the help of overseas training and collaboration of doctors working in the same field throughout Asia (40). Currently, transplant centers in Taiwan are helping in the diffusion of knowledge by providing training opportunities for doctors from various continents, and actively helping establishment of many transplant centers overseas. Notwithstanding its small size, LDLT has flourished in Taiwan on the basis of continuous innovations, education and enlightened guidelines. It is possible for developing countries to establish transplant programs that are successful in the long term by keeping these factors in mind while committing to a capital and labor intensive venture such as LT.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Chen CL, Kabiling CS, Concejero AM. Why does living donor liver transplantation flourish in Asia? Nat Rev Gastroenterol Hepatol 2013;10:746-51. [PubMed]
- Chen CL, Concejero AM, Cheng YF. More than a quarter of a century of liver transplantation in Kaohsiung Chang Gung Memorial Hospital. Clin Transpl 2011.213-21. [PubMed]
- Starzl TE. The puzzle people: Memoirs of a Transplant Surgeon. University of Pittsburgh. Pittsburgh,1992.
- Wait S, Chen DS. Towards the eradication of hepatitis B in Taiwan. Kaohsiung J Med Sci 2012;28:1-9. [PubMed]
- Lee MH, Yang HI, Yuan Y, et al. Epidemiology and natural history of hepatitis C virus infection. World J Gastroenterol 2014;20:9270-80. [PubMed]
- Sun CA, Chen HC, Lu CF, et al. Transmission of hepatitis C virus in Taiwan: prevalence and risk factors based on a nationwide survey. J Med Virol 1999;59:290-6. [PubMed]
- Lee MH, Yang HI, Jen CL, et al. Community and personal risk factors for hepatitis C virus infection: a survey of 23,820 residents in Taiwan in 1991-2. Gut 2011;60:688-94. [PubMed]
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010;127:2893-917. [PubMed]
- Chen CL, Wang KL, Lee MC, et al. Liver transplantation for Wilson’s disease -- Report of the first successful liver transplant in Taiwan. Jpn J Transplant 1987;22:178-84.
- de Villa VH, Chen CL, Chen YS, et al. International sharing of split liver grafts in Asia: initial experience. Clin Transplant 2000;14:355-9. [PubMed]
- Kawarasaki H, Iwanaka T, Nakajo T, et al. Live related partial liver transplantation with monkeys and clinical report of two cases. Japanese Journal of Pediatric Surgery 1990;22:966-73.
- Kawarasaki H, Iwanaka T, Tsuchida Y, et al. Partial liver transplantation from a living donor: experimental research and clinical experience. J Pediatr Surg 1994;29:518-22. [PubMed]
- Chen CL, Concejero A, Wang CC, et al. Living donor liver transplantation for biliary atresia: a single-center experience with first 100 cases. Am J Transplant 2006;6:2672-9. [PubMed]
- Lu CH, Tsang LL, Huang TL, et al. Biliary complications and management in pediatric living donor liver transplantation for underlying biliary atresia. Transplant Proc 2012;44:476-7. [PubMed]
- Cheng YF, Chen CL, Huang TL, et al. Single imaging modality evaluation of living donors in liver transplantation: magnetic resonance imaging. Transplantation 2001;72:1527-33. [PubMed]
- Jawan B, de Villa V, Luk HN, et al. Perioperative normovolemic anemia is safe in pediatric living-donor liver transplantation. Transplantation 2004;77:1394-8. [PubMed]
- Chen CL, Chen YS, de Villa VH, et al. Minimal blood loss living donor hepatectomy. Transplantation 2000;69:2580-6. [PubMed]
- Yang CH, Chen CL, Wang CC, et al. Dual grafts in adult-to-adult living donor liver transplantation: a single center experience in Taiwan. Surgery 2009;145:212-8. [PubMed]
- Sun CK, Chen CL, Concejero AM, et al. Retransplantation for end-stage liver disease: a single-center Asian experience. Transplant Proc 2008;40:2503-6. [PubMed]
- Cheng YF, Chen YS, Huang TL, et al. Interventional radiologic procedures in liver transplantation. Transpl Int 2001;14:223-9. [PubMed]
- Cheng YF, Ou HY, Tsang LL, et al. Interventional percutaneous trans-splenic approach in the management of portal venous occlusion after living donor liver transplantation. Liver Transpl 2009;15:1378-80. [PubMed]
- Cheng Y, Chen C, Lai CY, et al. Assessment of donor fatty livers for liver transplantation. Transplantation 2001;71:1221. Transplantation 2001;71:1206-7. [PubMed]
- Chen CL, Yap AQ, Concejero AM, et al. All-in-one sleeve patch graft venoplasty for multiple hepatic vein reconstruction in living donor liver transplantation. HPB (Oxford) 2012;14:274-8. [PubMed]
- de Villa VH, Chen CL, Chen YS, et al. Outflow tract reconstruction in living donor liver transplantation. Transplantation 2000;70:1604-8. [PubMed]
- Julka KD, Lin TS, Chen CL, et al. Reconstructing single hepatic artery with two arterial stumps: biliary complications in pediatric living donor liver transplantation. Pediatr Surg Int 2014;30:39-46. [PubMed]
- Li WF, Lin TS, Chen CL, et al. Using ileocolic artery for successful graft salvage in a recipient with hepatic artery thrombosis after living donor liver transplantation: case report. Transplant Proc 2012;44:581-2. [PubMed]
- Takatsuki M, Chiang YC, Lin TS, et al. Anatomical and technical aspects of hepatic artery reconstruction in living donor liver transplantation. Surgery 2006;140:824-8; discussion 829. [PubMed]
- Lin TS, Chen CL, Concejero AM, et al. Early and long-term results of routine microsurgical biliary reconstruction in living donor liver transplantation. Liver Transpl 2013;19:207-14. [PubMed]
- Wang CC, Lin TS, Chen CL, et al. Arterial reconstruction in hepatic artery occlusions in adult living donor liver transplantation using gastric vessels. Surgery 2008;143:686-90. [PubMed]
- Lin CC, Chuang FR, Lee CH, et al. The renal-sparing efficacy of basiliximab in adult living donor liver transplantation. Liver Transpl 2005;11:1258-64. [PubMed]
- Chen YS, Wang CC, de Villa VH, et al. Prevention of de novo hepatitis B virus infection in living donor liver transplantation using hepatitis B core antibody positive donors. Clin Transplant 2002;16:405-9. [PubMed]
- Hu TH, Chen CL, Lin CC, et al. Section 14. Combination of entecavir plus low-dose on-demand hepatitis B immunoglobulin is effective with very low hepatitis B recurrence after liver transplantation. Transplantation 2014;97:S53-9. [PubMed]
- Yao FY, Ferrell L, Bass NM, et al. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology 2001;33:1394-403. [PubMed]
- Sun PL, Chen CL, Hsu SL, et al. The significance of transarterial embolization for advanced hepatocellular carcinoma in liver transplantation. Transplant Proc 2004;36:2295-6. [PubMed]
- Yu CY, Ou HY, Huang TL, et al. Hepatocellular carcinoma downstaging in liver transplantation. Transplant Proc 2012;44:412-4. [PubMed]
- Liver transplant outcomes, Taiwan National Health Insurance; 2014 [cited 2015 15th March]. Available from: http://www.nhi.gov.tw/information/NewsDetail.aspx?menu=9&menu_id=544&No=1165
- Cheng YF, Ou HY, Yu CY, et al. Interventional radiology in living donor liver transplant. World J Gastroenterol 2014;20:6221-5. [PubMed]
- Chang CH, Lin JW, Wu LC, et al. National antiviral treatment program and the incidence of hepatocellular carcinoma and associated mortality in Taiwan: a preliminary report. Med Care 2013;51:908-13. [PubMed]
- Kabiling CS, Chen CL, Concejero A, et al. Section 18. Professional framework for liver transplantation for overseas patients: traveling for living donor liver transplantation. Transplantation 2014;97:S75-9. [PubMed]
- Chen CL. ' commentary: summit on living donor liver transplantation. Transplantation 2014;97:S2. [PubMed]


