Obesity, the deadly quartet and the contribution of the neglected daily organ rest - a new dimension of un-health and its prevention
Western life style and food habits - the real threat to health
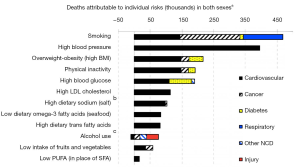
The epidemic of Western diseases is strongly associated with, in addition to stress and lack of exercise, overconsumption of processed Western type food, resulting in metabolic syndrome and manifested in what has been called the “deadly quartet”: excessive body weight, impaired glucose homeostasis, hypertension and atherogenic dyslipidemia- changes in serum cholesterol, increased triglycerides, decreased high density lipoprotein (HDL) cholesterol, and an increase of “small dense” low-density lipoprotein (LDL) particles], manifestations often followed by diseases such as diabetes mellitus type 2, cardiovascular disease (CVD), cancers such as breast, colorectal, pancreas, neurodegenerative diseases [e.g., Alzheimer’s disease (AD)], pregnancy complications (gestational diabetes, preeclampsia), fertility problems (polycystic ovarian syndrome) and much more. The development of metabolic syndrome with its ingredients: abdominal obesity, high blood pressure, elevated blood sugar, elevated blood triglycerides, low HDL cholesterols, high uric acid in blood is often, if not always, a result of malfunctioning gut flora (dysbiosis), induced endotoxemia, low grade systemic inflammation, malfunctioning immune system (1,2) - all constituting, what I call a “mother of disease” (3) (Figure 1) (4).
Early warnings should not be ignored
The dysbiosis-induced low-grade inflammation and malfunctioning immune system induces early a series of various, seemingly benign, manifestations in the body, for which the sufferers often seek medical advice at their local general practitioneer (GP, family doctor), and often receive symptomatic treatment. However, these minor, but irritating, symptoms should be taken seriously as they are all signs of ongoing low grade inflammation, which with time might bring serious consequences - severe diseases and with time death. Such signals should be regarded as “early warnings” and stimulate to radical changes in lifestyle and especially in food habits. Among these “early warnings” are manifestations such as: acne, dandruff, unexplained fatigue, sleep problems, frequent headache, hair loss, gray hair, skin rashes, dry eyes, frail nails, dry mouth or increased salivation, reduced sex functions, irregular menstruations, obstipation or diarrhea, osteoporosis, overweight, frequent infections, mental depression, easy breathless, sweaty feet, sweaty hand palms, vaginal flour - all accompanied by discrete increased low grade inflammation. If ignored - worse is to come.
Worse is to come
A series of professionally done studies suggest that most of the endemic chronic diseases, all from attention deficit hyperactivity disorder (ADHD), Alzheimer, and diabetes to prostatic and other cancers will in average be trippled in incidence by the year 2050: diabetes at least doubled (5) and the incidences of ADHD, Alzheimer disease (6) and cancer (7) at least tripled. No health insurance system, governmental orprivate, will have a chance to sustain under such conditions. Even at times with low inflation seems the cost for healthcare double each 10-year period (8). It can be calculated that in the USA, the country with the highest healthcare costs in the world, will by the year 2020: the costs of healthcare correspond to half (>$15,000) of the average family income (about $46,000) after tax (app 30,000) - sales tax excluded.
A rather recent and most interesting study looked at the prognosis for the USA and UK, together (9), two countries, which already have among the highest rates of obesity and chronic diseases in the world, and representing approximately 5% of the world’s population. The study suggests that these countries combined, by the year of 2030, will see another 76 million obese adults, and suffer from an additional 6-8.5 million cases of diabetes, 6-7 million cases of CVD, 492,000-669,000 cases of cancer, which would result in a loss of between 26 and 55 million quality-adjusted life years and a dramatic increase in costs of care, by the authors calculated to be $50-68 billion per year) (9).
The problem - easy access to food and to high consumption of processed foods
For some decades the epidemic of obesity and chronic diseases was mainly a problem for the Western world. Modern agricultural techniques, techniques for mass production and easy access of cheap foods has led to a much too large consumption of agricultural foods, especially industrially manipulated foods rich in processed agricultural products such as meat, dairy and wheat (10-12). Similar developments are now observed also in other parts of the world, largely in parallel to the adoption of a “modern”/Western lifestyle. Seemingly the epidemic of obesity and associated diseases has its epicenter in Southern USA (13), states like Alabama, Louisiana and Mississippi having the highest incidence of obesity and chronic diseases in the USA and the world. These diseases are spreading around the world much like a tsunami; to the West to New Zeeland and Australia, to the North to Canada, to both Eastern and Western Europe and now also to the Arab world and all Asian Countries and to the South, particularly Mexico and Brazil.
Now reaching Asia and Africa with a speed like a typhoon
Japan seems to have been the first country after what is called Western countries to adapt Western lifestyle and it suffers now the burden of Western diseases - to an extent rarely seen before. The island Okinawa, once said to have the best health and the greatest numbers of centenarians in the world, has after the USA did build military bases on the island and the island became westernized lost its leading position as the prefecture (state) with the lowest incidence of obesity, chronic diseases and number of centenarians in the world - today it ranks among the lowest when the 50 Japanese states (prefectures) are studied.
The death rate in prostatic cancer increased 25-fold during 50 years after the world war [1947-1998], when Japan, at least to some extent, adopted its food habits to Western agriculture-based foods, which happened in parallel to the increase in consumption of intake of eggs 7-fold, meat 9-fold and cow’s milk products 20-fold (14,15). Now the same development is seen in China, India and other Asian but also in African countries. China for example, once known for its extremely good lifestyle and food habits, especially in rural areas, and low incidence of obesity as well as chronic diseases but also high numbers of centenarians (16) is today badly affected by obesity and illness, also here much in parallel to introduction of Western type and especially with dramatically increased production and consumption of dairy products. I have had difficulties to access official information, but my professional colleagues tells, that the incidence of chronic diseases such as coronary heart diseases, diabetes, and cancers such as breast cancer and prostatic cancers seems to double each 10 years, especially observed in the large cities.
Incidence of obesity and chronic disease increases with unprecedented speed
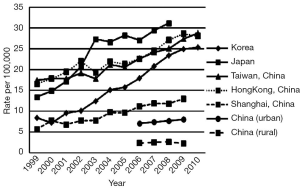
It is recently reported that the incidence of metabolic syndrome and cardiovascular risk rose dramatically in the Chinese population during only 8 recent years between the 2002 and 2010 (17). A 4-fold increase in incidence of metabolic syndrome was observed, affecting only 5.4% of the population in 2002 rising to as much as 21.3% in 2010. The situation seems even more serious considering that the rate of hyperglycemia rose 5 times, from 9.1% in 2002 to 53.1% in 2010. And, the age-standardized prevalence of obesity did double during the same period - from 13.5% to 25.4%, in parallel with increased incidence in hypertension (from 23.6% to 40.8%), hypertriglyceridemia (from 12.1% to 17.4%) and an alarming rise in low density cholesterol LDL (from 32.1% to 71.1%). It was also reported that the gap in incidence of metabolic syndrome and its serious consequences, previously much in favor of rural compared to urban populations decreased significantly during these 8 years (17). A just published study reports much similar development in cancer disease in South East Asia - exemplified by prostatic cancer, which is fast increasing; already high in Japan, Taiwan, Hong Kong and Korea, but also Shanghai and most likely also Beijing - but also urban China is fast following in the footprints of the most affected (Figure 2) (18). It is especially worrisome that the increase of Western habits is increasing considerably faster among the young Chinese. The metabolic syndrome and obesity is increasing faster in younger age groups and the prevalence of juvenile type 2 diabetes reported to have doubled within a recent 5 years period and today to have surpassed the prevalence of juvenile type 1 diabetes in other countries in Southeast Asia.
The interval between change of lifestyle and signs of un-health shorter than ever seen
It is of the greatest interest to observe that the interval between change of lifestyle and altered pattern of disease is much shorter than previously believed. What took about 100 years to occur in the Western world was obviously achieved in South East Asia in less than 10 years. The large increase in dairy production and consumption which exploded after the shift of millennium was seemingly almost immediately followed by a typhoon of obesity and chronic disease. Feeding large populations with cheap foods is obviously one of the greatest political problems, and measures to reduce this threat should be given high priority in all countries. Western politicians know well the consequences and have done so for decades but seemingly abstained from more serious attempts to stop the epidemic of obesity and chronic diseases which follows - they are obviously willing to accept the negative consequences and show little enthusiasm to stop this health-damaging development. Both in Europe and in the USA do governments continue to subsidize agriculture with large sums of money in order to stimulate increased production of foods, that when consumed in larger quantities will induce disease. They seem prepared to accept the large and fast increasing costs that follow to attempt to cure those, who have been affected by disease, induced by overconsumption of cheap calorie-condensed agricultural foods. Serious attempts to introduce large-scale preventive medicine has this far not been done in any country.
Consumption of refined sugar, strongly associated with obesity and Western diseases, has sky-rocketed in the last 150 years from a decent 1/2 kg in 1850 to presently about 50 kg/person/year in Western and South American countries. The consumption of sugar is still comparatively low in Asian countries - usually below 10 kg/person/year, but is fast growing. Despite the fact that Asian countries in addition to having a considerable internal and fast-growing production are India and China the largest importers of sugar in the world - China is expected to be the largest importer in the world in the year 2020. One can only speculate about the damaging effects on public health such a development will lead to.
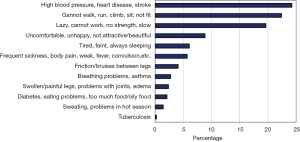
Also Africa is following on the same pathway - a recent study reports fast increasing public health problems with obesity in Tanzanian women with damaging physical and social consequences - the prevalence of overweight reported as considerable for the continent: 16% overweight, and 6% obese (Figure 3) (19).
Obesity - a complex issue
Clearly, obesity is a result of eating too much of the wrong foods - mainly refined industrially processed agriculturally produced foods, but there are other contributory factors which do not receive the attention that they should.
Among these factors are:
The importance of complying the “built-in” diurnal clock
Human beings are diurnal creatures. We conduct most of our activities during the day, including our feeding, our physical exercise and our work - the night is intended for relaxation and rest, not only our muscles but also our internal organs should be allowed to rest. It is a period aimed for recuperation, cleansing/detoxification and resetting of our various metabolic, immunological and other internal clocks, sometimes referred to as the period of resynchronization. These important processes were absolutely normal to our Paleolithic forefathers and to early generations of farmers and hunters, who normally rose with the sun and went to bed soon after the dawn, and they still are in cultures living a similar life as our forefathers. The urban lifestyle in modern societies is much different with all its negative consequences. Night activities are increasingly common: shift work, overtime work, night eating, sleep disruption and deprivation constitute a great threat to our normal diurnal rhythms and disrupt our metabolic clock and energy homeostasis. Increasing evidence suggests that for example shift workers have a higher risk of metabolic diseases, including obesity, diabetes, metabolic syndromes and CVDs and also that sleep deprivation, irregular sleep, sleep disruption and nightly meals have similar consequences (22-24).
Rest, recuperation, cleansing, detoxification - especially important in patients suffering early Alzheimer, diabetes, and fatty livers
Daily nocturnal fasting is important in order to reduce/eliminate poisonous substances from blood and tissues. Alzheimer’s disease (AD) is characterized by toxic accumulation in the brain amyloid beta (Aβ), induced by either overproduction or some clearance failure, and suggested to be the underlying mechanism of the neuronal cell death. Sleep disturbances are common early in various forms of dementia and other forms of neurodegenerative diseases, particularly in Alzheimer’s in early as well as in later stages (25). Sleep may play an important role in Aβ clearance, and getting good quality sleep reduces the AD risk associated with neuro-inflammation and the ε4 allele. It is recently reported that men, who suffer of sleep disturbances at an age of 70 years had an increase in general dementia with +114% and in AD with as much as +192% (both P<0.001) (26). Similar developments are recently reported in Parkinson’s disease (27), multiple sclerosis (28,29), epilepsy and other seizure disorders (29), amyotrophic lateral sclerosis (ALS) (30), Huntington’s disease (31) restless legs (29), obstructive sleep apnea (29) etc. Disturbances in the light/dark cycle, sleep/wake schedule, or feeding/activity behavior, disturbed circadian function of the diurnal clocks in various peripheral tissues and synchronized by the brain are strongly associated with impaired glucose tolerance especially in type 2 diabetes (32), changes beautifully illustrated in experimental studies (33).
The same group of researchers did also report the physiological consequences of Time-restricted feeding as observed in experiments in mice. Two groups of animals received exactly the same food and the same amounts of calories. One group was allowed to consume freely day and night, the other had it restricted to only half of the 24-hour day. Dramatic differences were observed in body weight, glucose intolerance (insulin resistance), leptin resistance, liver pathology (fatty infiltration) inflammation and motor coordination (33).
Paleolithic lifestyle stimulates a robust circadian rhythm & a healthy and long-lasting life
Observations that our forefathers might have eaten only twice a day are supported by studies in people with similar lifestyle. One such group is the Hunzas in Northern Pakistan, today known for their good health and high numbers of centenarians. The adult Hunzas are reported to live on a daily 1,800-calory 99% plant-based diet, consisting in 73% of mostly unrefined/unprocessed carbohydrates, 17% fat and 10% protein (34). They are going out to work in the fields around 5 o’clock in the moring with an empty stomach, and eat their main meal of the day at noon and a lighter meal just before going to bed around dawn - see further http://thepdi.com/hunza_health_secrets.htm and http://projectavalon.net/forum4/showthread.php?48210-HUNZAS-a-people-who-live-to-age-145-.
The concept of CR is not new, it was promoted already by ancient Greek medicine by giants such as Hippocrates, Galenus and later also Paracelsus. Louis Cornado [1464-1566] in his book La Vita Sobra, written when he was more than 80 years old, recommended in addition to a tranquil life and plenty of sleep and 1/2 l/d new/virgin/fresh red wine per day a diet consisting in at most 1/2 a kg of mainly fruits and vegetables, olive oil, a little bread and egg and occasionally a little fish and lean meat. He lived until an age of 102 years and his teaching influenced many generations during following centuries.
Calorie-restriction (CR) and time-restricted eating (TR) has not become a success
Most human studies aimed to compare health consequences of breakfast eating with those of no breakfast eating are unfortunately of rather poor quality as the period of metabolic rest varies conciderably. For example one individual might have the last meals at midnight and then consumes breakfast at 5:00 AM (providing only 5 hours overnight fast) while another BF-eater might have the last meal already at 6 PM and a late breakfast at 10 AM, providing 16 hours of “stomach rest” - both still concidered as BF-eaters (35).
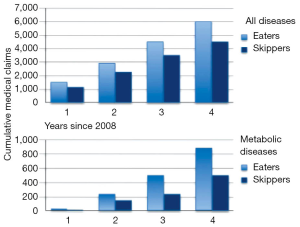
The compliance of the participants has often been low, and there has been a tendency towards compensatory eating during the following day often observed. It seems that the clinical effects are most effective when applied to middle-age people compared to younger or older. It is clearly documented that abstaining from late eating is more effective than abstaining from eating breakfast. It should be said, however, that almost all successful methods for reducing weight is without doubt reducing the size of the meals and changing the content towards mainly plant fibers eaten in the morning will not be metabolized during the closest 2-3 hours, which is the time needed for this food to be transported to the large intestine and to be metabolized by microbiota. Zilberter & Zilberter summarizes in a recent review the clinical effects of “skipping breakfast” as demonstrated on Figure 4 and mainly based by studies of Okamoto et al. (36) - a Japanese publication, which is difficult to find but most interesting to read. These authors followed during 53 months in the period 2008−2012 no less than 12,304 patients. The main conclusion from the analysis of Zilberter & Zilberter is that breakfast eaters and late eaters are more affected by disease and require more medical attendance than breakfast skippers and early evening eaters.
Postprandial inflammation of Western foods - a great burden to the immune system
Processed industrially produced Western foods are much richer in calories particularly agriculture derived sugar and sugar-like foods (bread, pasta, pizza, cooked tubers, polished rice etc.) and refined dairy products, rich in long-chain fatty acids. Sugar and sugar-like foods are absorbed by the small intestine within short time after intake and create during a 2-3 hours an increased burden to internal organs, in association with postprandial inflammation, and particularly affecting the liver.
The body has no possibility to take up long-chain fatty acids directly through the portal vein in order to be quickly metabolized - that is restricted to fatty acids with chain-length shorter than C12 (37). Long-chained fatty acids, to about 80% consisting in cow’s fat need to be transported by the thoracic duct via the general circulation to the liver. Most of it will remain in the general circulation during several hours and will expose the content of fat to the endothelium in various parts of the body including the carotids and the brain vessels, induce inflammation and intimal calcifications, known as strong risk factors in atherosclerosis and other chronic diseases such as Alzheimer’s and type 2 diabetes. Other consequences associated with elevated postprandial glucose and insulin concentrations are:
The obvious negative effects of consuming energy-rich foods were rarely observed before the Industrial Revolution and introduction of Western food habits - at least not to the same extent as today. The situation has dramatically become worse with introduction of sugar additives such as sucrose and high fructose corn syrup, today available in a large quantities in beverages and processed foods. Food ingredients supplied by larger meals, elevates both blood glucose and blood fat concentration, which is a risk to the individual - it must be kept within narrow limits for the individual to stay healthy.
The liver and skeletal muscles in focus
Non-alcoholic fatty liver disease (NAFLD) is today a most common chronic liver disease both in adults and children (41) and strongly associated with obesity, chronic liver diseases, diabetes and other chronic diseases. Fructose-induced lipogenesis is reported to be responsible for 26% of accumulated hepatic triglycerides and 15-23% of secreted very LDL triglycerides in patients with NAFLD compared to less than 5% in healthy subjects (42,43). Metabolic syndrome is today increasingly common in children and childhood NAFLD has become in recent years a highly prevalent childhood liver disease.
It has long been neglected, that skeletal muscle, is not only a part of our locomotor system, but also an important metabolic and also endocrine organ - as a matter of fact it constitutes approximately 45% of the total body mass and, furthermore, no less than 2,300 of skeletal muscle genes are involved in processes under control of circadian rhythms-involved in numerous metabolic processes including myogenesis, transcription, and metabolism (44). The skeletal muscle is the major storage of amino acids and sugars as glycogen (easy access energy) but not of fat. In humans 5 times more glycogen is stored in skeletal muscles (~500 g) compared to the liver (~100 g). Glycogen makes up about 1-2% of muscle weight and 6-10% of liver weight. The liver seems more willing to release its glycogen than the muscles, the content of which decreases more rapidly during fasting, when the liver glycogen content is decreased by ~65% after 24 hours fasting. In contrast, no major decrease is observed in muscle glycogen content during 24-hour fasting (44). It also takes some time, about 15-20 hours, before a considerable lipolysis starts in skeletal muscles (45).
Fatty infiltration of skeletal muscles, liver & some other organs-a sign of sickness
It is a sign of sickness that fat is stored in the liver and in skeletal muscles. Fatty infiltration is a sign of excessive consumption of foods or force-feeding of domestic animals with more or less unsuitable feeds and also influenced by physical inactivity. The meat produced by modern agriculture is of those reasons rich in fatty infiltration of skeletal muscles and of organs like the liver, and especially so in foods like goose liver pâté and pig meat. Changes in muscle composition and function are also strongly correlated with disease development. Recent studies demonstrate that disruptions in circadian rhythms will have detrimental effects to both skeletal muscle and general health. Chronic diseases, like arteriosclerosis, diabetes type 2 and others are intricately tied to skeletal muscle dysfunction (46).
Parker demonstrated more than 50 years ago in a now classical animal study that environmental poisons like diklordifenyltrikloretan (DDT) accumulate in the adipose tissues (47). Another by now classical study reported in 1972 the presence of phthalate ester plasticizer originating from the polyvinyl chloride blood bags in its content, human blood, aimed to be infused into the patient (48). Today most of the food we eat such as milk and juice have been stored in containers with plastic material on its inside. The fish we eat contains more or less of environmental chemicals and the meat often remnants of antibiotics, other drugs and various chemicals. Most of these are lipophilic and follows fats into the adipose tissues. Also endotoxin and remnants of various bacteria are ending up in the adipose tissues. Patients exposed to regular maintenance hemodialysis are reported to suffer high degree of inflammation and what has been called “paradox obesity” most likely due to sequestration of uremic and other toxic substances in adipose tissue.
Adipose tissue a “garbage bin” - inducing inflammation, further obesity and chronic diseases
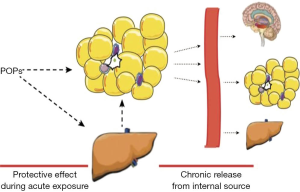
The adipose tissue is a complex organ with numerous endocrine, metabolic and immunological functions - but it is also, as mentioned above a storage of various inflammation-inducing toxins (49). The content in adipose tissues of persistent organic pollutants (POPs) - altogether 17 dioxins/furans and 18 polychlorinated biphenyl congeners, has been reported to be 2-3 times higher in obese compared to lean persons (50). The adipose tissues are, as a consequence of the accumulation POPs, infiltrated by macrophages, leukocytes, and activated natural killer T cells, and regulatory T cells, much in parallel to activation of bioactive molecules, collectively termed adipokines - processes leading to long-term inflammation and risk of chronic diseases. An unfortunate consequence is that the turnover of the fat in such conditions is significantly reduced - most likely in attempt to protect other, eventually more sensitive, tissues from further exposure to the toxins (Figure 5) (51).
Visceral adiposity - a greater problem than abdominal
Clearly the visceral adiposity which is common today did not exists among our Paleolithic forefathers - it is a phenomenon closely associated with overeating of processed calorie-condensed food, a possibility that did not exist in those days. Visceral fat should normally consist only in a few milliliters. Today, however, studies have demonstrated up to 6 litres of depot fat intraabdominally in extreme obesity (52). The fat localized in the abdomen is supposed to provide fast available extra calories in situations of acute stress in addition to release of proinflammatory factors such as IL-6 and PAI-1, which are released in amounts about three times as much per gram tissue compared to subcutaneous fat (53). The high amount of fatty acids and proinflammatory factors released in obese individuals in stressful situation do often create problems as they are associated with exaggerated inflammation and progress of disease (2,54-56).
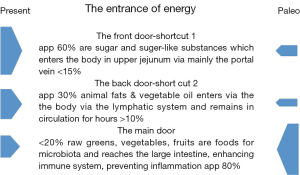
The processed and calorie-rich food that an increasing proportion of global inhabitants, consume creates unsolvable problems without considerable changes in diet habits. While Paleolithic food is estimated to consist in about 80% plant fibers - favored food for gut microbiota - modern human foods is estimated to contain less than 20% (Figure 6). A common recommendation of consumption of plant fiber based on epidemiologic studies, made both by nutrition organizations and governmental authorities is 25 g dietary fiber for adult women and 38 g for adult men. However the experience is that the common diet both in North America and Europe contains only around half that much, while the Hunzas, much like our Paleolithic forefathers, consume between 80 and 100 grams per day. It is certainly even more damaging that about 60% of consumed food in the West consists in sugar and “sugar-like” substances, which constitute an enormous burden to metabolic organ such as the liver, pancreas and also to the kidneys. It is also damaging that Western food is so rich in long-chain fatty acids, about 30% compared to less than 10% in Paleolithic food. As already emphasized, long-chain fatty acids enters the body through the thoracic duct and remain in circulation for hours before finally being metabolized by the liver.
To achieve effective lipolysis - considerable fasting is needed
It is estimated that during rest and sleep only about 65 calories will be “burnt” and during the type of work, that most of people have today, not much more, about 85 calories/day. In order to burn only 300 calories one will need to run about 5 km or cycle 20 km-running marathon is estimated to utilize not much than what is normally consumed in one day, not much more than 3,000 calories. Much support that regular fasting should be a necessary ingredient in our daily life. Many religious groups incorporate periods of fasting into their rituals including Muslims, who fast from dawn until dusk during the month of Ramadan, and Christians, Jews, Buddhists and Hindus who traditionally fast on designated days of the week or calendar year. In many medical clinics, patients are now monitored by physicians while undergoing “water only” or very low calorie (less than 200 kcal/day) fasting periods lasting from 1 week or longer for weight management, and for disease prevention and treatment - and impressive improvements in health are observed (57). A more effective but also more difficult to practice method is calorie restriction - e.g., reduction of the daily intake by 20-40% year around, which have demonstrated dramatic improvements in health (57). Daily fasting consisting in 16 to 18 hours by avoiding calorie intake between 18:00 in the evening and 10:00 or 12:00 AM. offers an attractive alternative, which I personally have practiced during many years.
Acknowledgements
None.
Footnote
Conflicts of Interest: Figure 5 is reproduced with permission from Environmental Health Perspectives and cited in the text.
References
- Bengmark S. Nutrition of the critically ill - emphasis on liver and pancreas. HepatoBiliary Surg Nutr 2012;1:25-52. [PubMed]
- Bengmark S. Gut microbiota, immune development and function. Pharmacol Res 2013;69:87-113. [PubMed]
- Bengmark S. Acute and "chronic" phase reaction-a mother of disease. Clin Nutr 2004;23:1256-66. [PubMed]
- Danaei G, Ding EL, Mozaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med 2009;6:e1000058. [PubMed]
- Boyle JP, Thompson TJ, Gregg EW, et al. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr 2010;8:29. [PubMed]
- Hebert LE, Scherr PA, Bienias JL, et al. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol 2003;60:1119-22. [PubMed]
- Bray F, Møller B. Predicting the future burden of cancer. Nat Rev Cancer 2006;6:63-74. [PubMed]
- Heffler S, Smith S, Keehan S, et al. U.S. health spending projections for 2004-2014. Health Aff (Millwood) 2005.Suppl Web Exclusives:W5-74-W5-85. [PubMed]
- Wang YC, McPherson K, Marsh T, et al. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011;378:815-25. [PubMed]
- Bengmark S. Advanced glycation and lipoxidation end products--amplifiers of inflammation: the role of food. JPEN J Parenter Enteral Nutr 2007;31:430-40. [PubMed]
- Bengmark S. Age, ale rage and disease-a foods perspective. In: Susan S Cho, Terry Finocchiaro, editors. Handbook of Prebiotic and Probiotic Ingredients: Health Benefits and Food Applications. Boca Raton: CRC Press, Taylor and Francis Group, 2010:139-62.
- Bengmark S. Modified Amino Acid-Based Molecules: Accumulation and Health Implications. In: Mello JFD, editors. Amino Acids in Human Nutrition and Health. Cambridge: Wallingford, UK, 2011:382-405.
- Adult Obesity Facts. Available online: http://www.cdc.gov/obesity/data/adult.html
- Li XM, Ganmaa D, Sato A. The experience of Japan as a clue to the etiology of breast and ovarian cancers: relationship between death from both malignancies and dietary practices. Med Hypotheses 2003;60:268-75. [PubMed]
- Ganmaa D, Li XM, Wang J, et al. Incidence and mortality of testicular and prostatic cancers in relation to world dietary practices. Int J Cancer 2002;98:262-7. [PubMed]
- Campbell TC, Campbell TM. The China Study: The Most Comprehensive Study of Nutrition Ever Conducted and the Startling Implications for Diet, Weight Loss, and Long-term Health. Ben Bella Books, Dallas, USA, 2006.
- Lao XQ, Ma WJ, Sobko T, et al. Dramatic escalation in metabolic syndrome and cardiovascular risk in a Chinese population experiencing rapid economic development. BMC Public Health 2014;14:983. [PubMed]
- Zhu Y, Wang HK, Qu YY, et al. Prostate cancer in East Asia: evolving trend over the last decade. Asian J Androl 2015;17:48-57. [PubMed]
- Keding GB, Msuya JM, Maass BL, et al. Obesity as a public health problem among adult women in rural Tanzania. Glob Health Sci Pract 2013;1:359-71. [PubMed]
- Dhurandhar EJ, Keith SW. The aetiology of obesity beyond eating more and exercising less. Best Pract Res Clin Gastroenterol 2014;28:533-44. [PubMed]
- McAllister EJ, Dhurandhar NV, Keith SW, et al. Ten putative contributors to the obesity epidemic. Crit Rev Food Sci Nutr 2009;49:868-913. [PubMed]
- Huang W, Ramsey KM, Marcheva B, et al. Circadian rhythms, sleep, and metabolism. J Clin Invest 2011;121:2133-41. [PubMed]
- Wang XS, Armstrong ME, Cairns BJ, et al. Shift work and chronic disease: the epidemiological evidence. Occup Med (Lond) 2011;61:78-89. [PubMed]
- Kawabe Y, Nakamura Y, Kikuchi S, et al. Relationship between shift work and clustering of the metabolic syndrome diagnostic components. J Atheroscler Thromb 2014;21:703-11. [PubMed]
- Cipriani G, Lucetti C, Danti S, et al. Sleep disturbances and dementia. Psychogeriatrics 2015;15:65-74. [PubMed]
- Benedict C, Byberg L, Cedernaes J, et al. Self-reported sleep disturbance is associated with Alzheimer’s disease risk in men. Alzheimers Dement 2014. [Epub ahead of print]. [PubMed]
- Hu Y, Yu SY, Zuo LJ, et al. Parkinson disease with REM sleep behavior disorder: features, α-synuclein, and inflammation. Neurology 2015;84:888-94. [PubMed]
- Braley TJ, Segal BM, Chervin RD. Underrecognition of sleep disorders in patients with multiple sclerosis. J Clin Sleep Med 2015;11:81. [PubMed]
- Marrie RA, Reider N, Cohen J, et al. A systematic review of the incidence and prevalence of sleep disorders and seizure disorders in multiple sclerosis. Mult Scler 2015;21:342-9. [PubMed]
- Gaig C, Iranzo A. Sleep-disordered breathing in neurodegenerative diseases. Curr Neurol Neurosci Rep 2012;12:205-17. [PubMed]
- Videnovic A, Lazar AS, Barker RA, et al. ’The clocks that time us’--circadian rhythms in neurodegenerative disorders. Nat Rev Neurol 2014;10:683-93. [PubMed]
- Vieira E, Burris TP, Quesada I. Clock genes, pancreatic function, and diabetes. Trends Mol Med 2014;20:685-93. [PubMed]
- Chaix A, Zarrinpar A, Miu P, et al. Time-restricted feeding is a preventative and therapeutic intervention against diverse nutritional challenges. Cell Metab 2014;20:991-1005. [PubMed]
- Robbins J. Healthy at 100: The Scientifically Proven Secrets of the World’s Healthiest and Longest-Lived Peoples. Ballantine Books, Random House Group, New York, USA.
- Zilberter T, Zilberter EY. Breakfast: to skip or not to skip? Front Public Health 2014;2:59. [PubMed]
- Okamoto E, Hiratsuko Y, Otsubo K, et al. Evaluation of the health checkup and guidance program through linkage with health insurance claims. J Natl Public Health 2013;62:13-30.
- Ward D, English J. Beneficial Effects on Energy, Atherosclerosis and Aging. Available online: http://nutritionreview.org/2013/04/medium-chain-triglycerides-mcts/
- Erridge C, Attina T, Spickett CM, et al. A high-fat meal induces low-grade endotoxemia: evidence of a novel mechanism of postprandial inflammation. Am J Clin Nutr 2007;86:1286-92. [PubMed]
- Ceriello A, Quagliaro L, Piconi L, et al. Effect of postprandial hypertriglyceridemia and hyperglycemia on circulating adhesion molecules and oxidative stress generation and the possible role of simvastatin treatment. Diabetes 2004;53:701-10. [PubMed]
- Alipour A, van Oostrom AJ, Izraeljan A, et al. Leukocyte activation by triglyceride-rich lipoproteins. Arterioscler Thromb Vasc Biol 2008;28:792-7. [PubMed]
- Bray GA, Popkin BM. Dietary sugar and body weight: have we reached a crisis in the epidemic of obesity and diabetes?: health be damned! Pour on the sugar. Diabetes Care 2014;37:950-6. [PubMed]
- Vos MB, Lavine JE. Dietary fructose in nonalcoholic fatty liver disease. Hepatology 2013;57:2525-31. [PubMed]
- Lefta M, Wolff G, Esser KA. Circadian rhythms, the molecular clock, and skeletal muscle. Curr Top Dev Biol 2011;96:231-71. [PubMed]
- Vendelbo MH, Clasen BF, Treebak JT, et al. Insulin resistance after a 72-h fast is associated with impaired AS160 phosphorylation and accumulation of lipid and glycogen in human skeletal muscle. Am J Physiol Endocrinol Metab 2012;302:E190-200. [PubMed]
- Soeters MR, Soeters PB, Schooneman MG, et al. Adaptive reciprocity of lipid and glucose metabolism in human short-term starvation. Am J Physiol Endocrinol Metab 2012;303:E1397-407. [PubMed]
- Jensen J, Rustad PI, Kolnes AJ, et al. The role of skeletal muscle glycogen breakdown for regulation of insulin sensitivity by exercise. Front Physiol 2011;2:112. [PubMed]
- Parker VH. 1:1:1-Trichloro-2:2-di-(p-chlorophenyl)ethane (DDT) and rat adipose tissue. Biochem J 1960;77:74-8. [PubMed]
- Jaeger RJ, Rubin RJ. Migration of a phthalate ester plasticizer from polyvinyl chloride blood bags into stored human blood and its localization in human tissues. N Engl J Med 1972;287:1114-8. [PubMed]
- Kalantar-Zadeh K, Kopple JD. Obesity paradox in patients on maintenance dialysis. Contrib Nephrol 2006;151:57-69. [PubMed]
- La Merrill M, Emond C, Kim MJ, et al. Toxicological function of adipose tissue: focus on persistent organic pollutants. Environ Health Perspect 2013;121:162-9. [PubMed]
- Kim MJ, Marchand P, Henegar C, et al. Fate and complex pathogenic effects of dioxins and polychlorinated biphenyls in obese subjects before and after drastic weight loss. Environ Health Perspect 2011;119:377-83. [PubMed]
- Thomas EL, Saeed N, Hajnal JV, et al. Magnetic resonance imaging of total body fat. J Appl Physiol (1985) 1998;85:1778-85. [PubMed]
- Alessi MC, Peiretti F, Morange P, et al. Production of plasminogen activator inhibitor 1 by human adipose tissue: possible link between visceral fat accumulation and vascular disease. Diabetes 1997;46:860-7. [PubMed]
- Bengmark S. Bioecologic control of inflammation and infection in critical illness. Anesthesiol Clin 2006;24:299-323. vi. [PubMed]
- Bengmark S. Pro- and synbiotics to prevent sepsis in major surgery and severe emergencies. Nutrients 2012;4:91-111. [PubMed]
- Bengmark S. Nutrition of the critically ill — a 21st-century perspective. Nutrients 2013;5:162-207. [PubMed]
- Longo VD, Mattson MP. Fasting: molecular mechanisms and clinical applications. Cell Metab 2014;19:181-92. [PubMed]


