
Reply to: The letter to the editor “Laparoscopic liver resection for malignancies confined to Couinaud’s segment VII in the robotic surgery era” by Zizzo et al.—laparoscopic liver resection: a first choice for liver malignancies in Couinaud’s segment VII in the robotic surgery era
We are grateful for the comments of Maurizio Zizzo et al. referring to our review article focusing on the present and future of laparoscopic liver resection (LLR) (1). In fact, this comment and letter to the editor reflects the current debates on (I) the wide-spreading indication of LLR; (II) whether we should consider LLR as a first-choice for malignancies confined to segment VII; (III) the advantages and disadvantages of robotic hepatectomy.
Although the comments of Zizzo et al. are straight to the point and perfectly complete, please allow us to make further remarks: as stated by Zizzo et al., LLR is noninferior to open procedures for hepatic resections in the aspects of oncological and intraoperative/perioperative outcomes (2). With accumulation of experience and innovation of instruments and techniques, most previous limitations for LLR have been conquered, especially the segment VII tumors and cirrhotic liver. To ensure future liver remnant volume (>40%) for liver malignancies with cirrhosis, we can adopt the method of the associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) to attain rapid growth of remnant liver instead of liver transplantation. In our institute, Cai’s ALPPS (3) was developed, using laparoscopic round-the-liver ligation to substitute for liver splitting at first stage, which can reduce adhesion and avoid bile leakage. Of note, although liver cirrhosis was a negatively prognostic element for conversion and complication of LLR, using the novel scoring system developed by Tong et al. (4), we could predict the possibility of them preoperatively to understand the cost to benefit in LLR and recommend experienced surgeons.
Segment VII, the deepest region of liver, lies behind the flat defined by right hepatic vein (RHV) and the vena cava. Therefore, it is important for resection of segment VII malignancies to mobilize the right liver from the diaphragm, right adrenal gland, and vena cava by dividing inferior RHVs. The malignancies of segment VII consist of hepatocellular carcinoma (HCC) and colorectal liver metastasis (CRLM) and other rare diseases. And nonanatomic wedge resection (WR) is recommended in the treatment of the latter, while anatomic segmentectomy VII is for the former. Meanwhile, right lateral segmentectomy (RLS) and right hepatectomy (all anatomic) were indicated with the suspicion of tumor infiltration to the proximal Glissonian sheath.
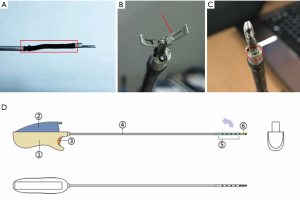
Currently, technical innovation, constantly updated surgical instruments, and experience accumulation have improved the safety, feasibility, and effectiveness of laparoscopic resection for Segment VII tumors. Fully preoperative assessment of accurate liver mass removed and residual liver volume (LV) using three-dimensional reconstruction enable to permit detailed reconstruction of the vascular and biliary anatomy of liver, and offer the potential to measure LV (5). Meanwhile, the combination of intraoperative ultrasonography (IOUS) (6) and fluorescence imaging system using indocyanine green (ICG) (7) is indispensable and it promotes the progress of LLR significantly depending on careful identification of hepatic veins and Glissonian system, and the boundary of segments, respectively. The approaches to posterosuperior segment (VII) have been multiple with different patient positioning. Fiorentini et al. (8) proposed a step-by-step guide to achieve a total transabdominal laparoscopic approach to segment VII. Instead of sacrificing the supine position and using intercostal and transthoracic ports, they adopted up-to-down mobilization, counterclockwise mobilization, and even flipping-over rotation to “commute” a posterosuperior segment (VII) into an anteroinferior position. In our institute, we developed laparoscopic Peng’s multifunctional operative surgical dissector (LPMOD), which has functions of dissection, cutting, aspiration and coagulation. And it is much easier for surgeons familiar with it to transect liver parenchyma and dissect small vessels inside liver parenchyma (9). Recently, a new laparoscopic surgical instrument with a flexible joint and elaborate camera in the distal, named visual multifunctional blunt separator, was invented to separate arterial branches towards segment VII and portal branch of the right lateral sector during hepatic hilum dissection and expose RHV as a landmark of the intrahepatic segmental boundaries (Figure 1). Furthermore, laparoscopic selective hepatic inflow occlusion plus portal vein occlusion (PVO) emerged recently in our institute, which avoids the ischemia-reperfusion injury and hemodynamic change.
With resection of Segment VII malignancies, Guerra et al. (10) do believe that operation may benefit greatly from robotic procedures. Firstly, 3-dimensional imaging, augmented surgical dexterity, and a global range of movements ensure accurate dissections. Moreover, Both the operative field and the fully robot-integrated ultrasonography are real-time, which help precise understanding of anatomy and vascularity and continuous dissections. Notably, all features above permit immediate processing of severe intraoperative complications. However, the non-negligible learning curve of da Vinci Surgical Systems must be respected, which may be a restrain of the development of robotic surgery. Although LLR seems to have a bottleneck in the period, thanks to the prevalence of LLR and basic technical skills acquired through a systematic and learning curve-based training course, the learning curve of sophisticated LLR, including surgery for segment VII malignancies, may become steeper in China in the near future.
In conclusion, for LLR of posterosuperior segment VII malignancies, the indications have been expanded. As technical innovation, instrument invention, steeper learning curves emerge, LLR for malignancies confined to Couinaud’s segment VII may be a first choice in the robotic surgery era.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Cai X. Laparoscopic liver resection: the current status and the future. Hepatobiliary Surg Nutr 2018;7:98-104. [Crossref] [PubMed]
- Ciria R, Cherqui D, Geller DA, et al. Comparative Short-term Benefits of Laparoscopic Liver Resection: 9000 Cases and Climbing. Ann Surg 2016;263:761-77. [Crossref] [PubMed]
- Cai X, Peng S, Duan L, et al. Completely laparoscopic ALPPS using round-the-liver ligation to replace parenchymal transection for a patient with multiple right liver cancers complicated with liver cirrhosis. J Laparoendosc Adv Surg Tech A 2014;24:883-6. [Crossref] [PubMed]
- Tong Y, Li Z, Ji L, et al. A novel scoring system for conversion and complication in laparoscopic liver resection. Hepatobiliary Surg Nutr 2018;7:454-65. [Crossref] [PubMed]
- Wigmore SJ, Redhead DN, Yan XJ, et al. Virtual hepatic resection using three-dimensional reconstruction of helical computed tomography angioportograms. Ann Surg 2001;233:221-6. [Crossref] [PubMed]
- Donadon M, Torzilli G. Intraoperative ultrasound in patients with hepatocellular carcinoma: from daily practice to future trends. Liver Cancer 2013;2:16-24. [Crossref] [PubMed]
- Berardi G, Wakabayashi G, Igarashi K, et al. Full Laparoscopic Anatomical Segment 8 Resection for Hepatocellular Carcinoma Using the Glissonian Approach with Indocyanine Green Dye Fluorescence. Ann Surg Oncol 2019;26:2577-8. [Crossref] [PubMed]
- Fiorentini G, Ratti F, Cipriani F, et al. Theory of Relativity for Posterosuperior Segments of the Liver. Ann Surg Oncol 2019;26:1149-57. [Crossref] [PubMed]
- Cai X, Duan L, Wang Y, et al. Laparoscopic hepatectomy by curettage and aspiration: a report of 855 cases. Surg Endosc 2016;30:2904-13. [Crossref] [PubMed]
- Guerra F, Bonapasta SA, Annecchiarico M, et al. Liver Malignancies in Segment VII: The Role of Robot-assisted Surgery. Ann Surg 2017;265:E80. [Crossref] [PubMed]


