
Difficulty scores in laparoscopic liver surgery—getting closer to a powerful and necessary tool
Obtaining standardized difficulty scores for surgical techniques is mandatory. The more accurate the scores become, the better results may be achieved in terms of patients’ safety and surgical implementation. This need is especially useful when technically demanding and complex surgical procedures are performed. In this sense, liver resections are difficult procedures with high morbidity and mortality rates that should be performed by experienced surgeons. Hepatobiliary surgery has always been considered as a long-term project that needs patience, expertise and a progressive learning curve. Since the first reported laparoscopic liver resection in 1996, the adoption and implementation of minimally invasive liver surgery has been cautious. However, laparoscopic liver resections have experienced a wide expansion in recent years (1), mainly after the last Consensus Meeting held in Morioka in 2014 (2). One of the statements reported during this Consensus and in the latter European Guidelines Meeting held in Southampton in 2017 (3) is that a need for a safe expansion and control on technical procedures should be encouraged. In this context, liver surgical teams are trying to develop feasible tools that may standardize laparoscopic liver resections.
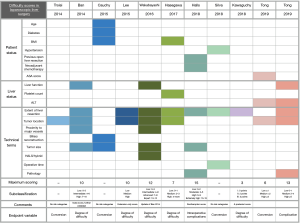
Some difficulty scores have been published and several variables have been reported to have an impact on surgical outcomes. Different endpoints (including postoperative complications, intraoperative difficulties and/or conversions) have been analyzed. Similarly, several variables including patient-, organ- and technical-related have been extensively included in the multivariate models (Figure 1). The recent manuscript from Tong et al. (4) has tried to arise a new score including conversions and complications as the main endpoints. As in most of the scores reported to date, patients’ variables are scarce and only anesthetic risk (ASA score) has been included in the conversion model. Interestingly, alanine aminotransferase (ALT) value as the only parameter regarding liver function has been included in this study and is the only score to date analyzing the impact of this value; this may need further evaluation in validation studies. The authors tried to perform an interim development/validation analysis comparing this new score with the currently reported ones in the literature. Although interesting, two main limitations should be noted: first, more than 85% of the resections were minor ones, leading to an unbalanced risk analysis that may turn into a bias; and second, the validation set was performed at the same institution, leading to potentially selection and analysis biases that may also have not been considered adequately.
Probably the score that has been studied in more depth is the Iwate score. This score was initially published in 2014 and updated in 2016 (5). A total of 6 variables makes this score the one that considers more variables and one of the two scores that includes 4 difficulty categories with an “expert” one for extremely complex cases. Although interesting and validated, it should be noted that this score is a technical score that considers no data from the patient’s status. Another well studied score in a large population dataset is the recently reported Southampton score (6). This score considered intraoperative events and complications as the main goal. It should be noted that this is the only score considering previous abdominal surgery and pre-operative neoadjuvant chemotherapy as important variables. Previous abdominal surgery leads to adhesions that may lead to severe complications including perforations and diffuse bleeding. Pre-operative neoadjuvant chemotherapy may make the liver become difficult to manipulate during the surgical procedure. A post-chemotherapy liver is soft and fragile leading to severe bleeding that could be difficult to control with standard maneuvers. In this context, sinusoidal obstruction syndrome is a hepatic veno-occlusive disease that increases bleeding despite Pringle and low-central venous pressure strategies during the laparoscopic procedure. These 2 subjective variables are important for liver surgeons and the authors should be congratulated for including them in their analysis.
Liver status has not been clearly included in any of the scores. In fact, the evaluation of liver function still needs consensus and agreement. All the scores reported to date consider anatomical liver variables but few of them consider functional status as a main variable. The extent of liver resection, posterior segments or proximity to major vessels are anatomical landmarks that consider only a “technically-based difficulty”. However, functional status of the liver is still underestimated in all scores reported to date. Probably, future complexity score may incorporate indocyanine green kinetics, nuclear imaging techniques as scintigraphy, or some other functional variables in the armamentarium. The impact of the cycles of intermittent clamping, duration of surgery or complexity of the resection balanced with liver function is still unknown and needs further evaluation.
Considering the trends of the population, we strongly believe that body mass index and cardiovascular/pulmonary co-morbidities have not been adequately balanced in the scores, and may strongly have an impact on intraoperative events or postoperative outcomes. Mainly in the western world, the connection between obesity, metabolic syndrome, fatty liver disease and hepatocellular carcinoma is well established. These parameters lead to extreme difficulty during the surgical procedure and further perioperative complications such as pneumonia, atelectasis, pulmonary embolism and impaired response to infectious complications. In the later setting, incisional hernias in the extraction area or disease recurrence may lead to reduced outcomes that have been underestimated with current scores. The recently reported score from Hasegawa et al. is the only score that includes body mass index (BMI), an indirect liver function variable (platelets), and two other technical variables (7).
The present and the immediate future of liver resections is based in minimally invasive techniques. However, it should be remarked that liver surgery needs precision, knowledge, expertise and a long learning curve in which complex open procedures are also included. New generations will surely perform some laparoscopic liver procedures without a previous open-learning curve, similarly to what has happened with cholecystectomy. However, difficulty scores are mandatory in order to adequately prepare trainees for a stepwise process in order to avoid complications or mortality. The perfect score has not been achieved yet, but is getting closer.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ciria R, Cherqui D, Geller DA, et al. Comparative Short-term Benefits of Laparoscopic Liver Resection: 9000 Cases and Climbing. Ann Surg 2016;263:761-77. [Crossref] [PubMed]
- Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 2015;261:619-29. [PubMed]
- Abu Hilal M, Aldrighetti L, Dagher I, et al. The Southampton Consensus Guidelines for Laparoscopic Liver Surgery: From Indication to Implementation. Ann Surg 2018;268:11-8. [Crossref] [PubMed]
- Tong Y, Li Z, Ji L, et al. A novel scoring system for conversion and complication in laparoscopic liver resection. Hepatobiliary Surg Nutr 2018;7:454-65. [Crossref] [PubMed]
- Wakabayashi G. What has changed after the Morioka consensus conference 2014 on laparoscopic liver resection? Hepatobiliary Surg Nutr 2016;5:281-9. [Crossref] [PubMed]
- Halls MC, Berardi G, Cipriani F, et al. Development and validation of a difficulty score to predict intraoperative complications during laparoscopic liver resection. Br J Surg 2018;105:1182-91. [Crossref] [PubMed]
- Hasegawa Y, Wakabayashi G, Nitta H, et al. A novel model for prediction of pure laparoscopic liver resection surgical difficulty. Surg Endosc 2017;31:5356-63. [Crossref] [PubMed]


