
Tumor progression in two-stage liver resections—is the shorter inter-stage period in associated liver partition and portal vein ligation for staged hepatectomy (ALPPS) of benefit to the patient?
A two-stage liver resection is a surgical option in patients with bilobar liver tumors in whom a single procedure is not feasible because of insufficient functional volume of the future liver remnant. The use of unilateral portal vein occlusion, such as portal vein embolization, induce hypertrophy of the future liver remnant in order to enable subsequent resection. Concomitant enhancement of tumor growth along with the hypertrophy response has raised concerns regarding oncological outcomes of the procedure. Therefore, the future liver remnant is generally cleared of all tumors during the first stage before portal vein occlusion is undertaken. Despite this approach, two-stage resection has been associated with a substantial drop-out rate due to tumor progression during the waiting time before the second stage. In traditional two-stage resection, the interval between stage 1 and 2 is usually 2–3 months (1). In recent years, associated liver partition and portal vein ligation for staged hepatectomy (ALPPS) has emerged as a new strategy to enhance hypertrophy of the future liver remnant. ALPPS entails a compressed version of the traditional two-stage procedure in which the inter-stage interval is much shorter owing to a much higher and faster hypertrophy response. In ALPPS, clearance of the future liver remnant is combined with portal vein occlusion (ligation or embolization) and partial or complete in situ split of the parenchyma during stage 1. Completion of the resection is performed during the second stage by removal of the deportalized liver after an interval of 1–2 weeks. ALPPS has raised a tremendous interest in the hepatobiliary surgical society, but also caused an on-going debate leading to some authors calling it the hepatopancreatobiliary (HPB) controversy of the decade (2).
While initial publications reported an unacceptably high mortality following this procedure, postoperative major morbidity has now dropped to acceptable levels with increased experience. Patients with colorectal liver metastases seemed to have a more favorable postoperative course compared to patients with primary hepatobiliary tumors operated with this technique. This was recently confirmed in the only randomized trial comparing conventional two-stage hepatectomy to ALPPS (3). Even if patients with colorectal liver metastases remain as a group where treatment with ALPPS has potential benefit, concerns persist regarding early disease recurrence and a too short inter-stage interval to be able to appropriately assess tumor progression (4).
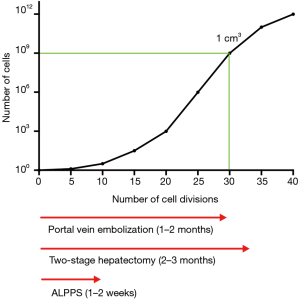
The inter-stage window in the ALPPS procedure might be too short to allow detection of new tumor manifestations. The kinetic development of micrometastases has been explored mathematically in order to estimate growth rates in different tumors types (5). If one assumes that colorectal liver metastases follow the same pattern requiring 30 volume doublings (109 cells or 1 cm3 of tumor mass) to be clinically detectable, the inter-stage interval of around 7–15 days reported in ALPPS will most certainly be too short to allow micrometastases to reveal themselves on modern radiological imaging (Figure 1). Accelerated tumor growth in the inter-stage period in two-stage hepatectomy and ALPPS have been explored in a murine model and in humans, and failed to show increased tumor growth in ALPPS (6). However, these studies do not address the potential micrometastases in the future liver remnant that remain undetected due to a short inter-stage period.
Whether a longer period between the two operations in ALPPS would result in overt tumor progression up to the point of unresectability is not known, since new tumor manifestations in the future liver remnant could also potentially be treated with curative intent. What is known from the two-stage hepatectomy setting is however, that about one third of the patients never proceed to the second operation, and that the main reason for this is tumor progression during the interval (typically around two months) between the two stages (7). One might speculate that part of these patients with incipient micrometastases in the future liver remnant would be left undetected if they had undergone ALPPS and that these lesions would appear as recurrences after completion of ALPPS.
So, the question about the optimal oncological strategy for these patients remains unanswered. Should we try to keep the interval between the two operations short to increase resection rates and later aim at treating recurrent metastases when they become manifest, or should we stick to the test-of-time with a longer inter-stage period in order to select patients that are more likely to benefit from hepatectomy? Studies focusing on long-term oncological outcomes after ALPPS are necessary to shed more light on this issue.
Acknowledgments
None
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Regimbeau JM, Cosse C, Kaiser G, et al. Feasibility, safety and efficacy of two-stage hepatectomy for bilobar liver metastases of colorectal cancer: a LiverMetSurvey analysis. HPB (Oxford) 2017;19:396-405. [Crossref] [PubMed]
- Olthof PB, Schnitzbauer AA, Schadde E. The HPB controversy of the decade: 2007-2017 - Ten years of ALPPS. Eur J Surg Oncol 2018;44:1624-7. [Crossref] [PubMed]
- Sandstrom P, Rosok BI, Sparrelid E, et al. ALPPS Improves Resectability Compared With Conventional Two-stage Hepatectomy in Patients With Advanced Colorectal Liver Metastasis: Results From a Scandinavian Multicenter Randomized Controlled Trial (LIGRO Trial). Ann Surg 2018;267:833-40. [Crossref] [PubMed]
- Olthof PB, Huiskens J, Wicherts DA, et al. Survival after associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) for advanced colorectal liver metastases: A case-matched comparison with palliative systemic therapy. Surgery 2017;161:909-19. [Crossref] [PubMed]
- Withers HR, Lee SP. Modeling growth kinetics and statistical distribution of oligometastases. Semin Radiat Oncol 2006;16:111-9. [Crossref] [PubMed]
- Kambakamba P, Linecker M, Schneider M, et al. Impact of associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) on growth of colorectal liver metastases. Surgery 2018;163:311-7. [Crossref] [PubMed]
- Vigano L, Torzilli G, Cimino M, et al. Drop-out between the two liver resections of two-stage hepatectomy. Patient selection or loss of chance? Eur J Surg Oncol 2016;42:1385-93. [Crossref] [PubMed]


