Nonalcoholic fatty liver disease: does sex matter?
Introduction
The hallmark of nonalcoholic fatty liver disease (NAFLD) is the intrahepatocyte accumulation of lipids with or without necro-inflammatory changes and ballooning [i.e., steatohepatitis or nonalcoholic steatohepatitis (NASH)], fibrosis, cirrhosis and hepatocellular carcinoma (HCC), which is observed in dysmetabolic individuals in the absence of competing causes of chronic liver disease such as excess alcohol consumption, viral infections, autoimmune or hereditary conditions and steatogenic medications (1). NAFLD represents an example of lipotoxicity caused by ectopic lipid accumulation. Even relatively modest amounts of ectopic lipid accumulation in normally lean organs (e.g., liver, pancreas, heart, kidney and muscle) can trigger functional disturbance in the affected organs and a subsequent vicious circle of adverse metabolic consequences in predisposed individuals (1); this will eventually result in those hepatic and extra-hepatic manifestations and co-morbid conditions which are frequently observed in NAFLD patients. Under this perspective, NAFLD should be viewed as one of the systemic manifestations and consequences resulting from lipid overflow.
NAFLD has been drawing major research as well as clinical interests due to (I) rapid epidemic diffusion and identification of the disease on a worldwide basis; (II) its mutual and bidirectional relationship with features of the metabolic syndrome; (III) strong (potentially causal) association with cardiovascular events; (IV) its escalating prevalence as a cause of chronic liver disease, cirrhosis, HCC and liver transplantation; and (V) on the grounds of all the reasons listed above, its posing a major burden on public health budgets in many countries of the world (1).
Although the term of ‘nonalcoholic steatohepatitis’ first coined in 1980 by Ludwig with a double composite word, which is typically German, what we now call NASH was probably reported in 1962 by Thaler and liver disease in the obese was recognized as early as 1952 by Zelman (2). So, what is left obscure after almost 70 years of explosive and ever progressing research on NAFLD and NASH?
The paper by Friedman and colleagues
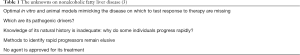
Doctors Friedman and colleagues recently published a review article which summarizes comprehensive state-of-the-art knowledge of NAFLD, covering from epidemiology, current and projected disease burden, histological features and pathogenesis, current therapeutic targets and their pitfalls, available experimental models to current challenges in clinical trials. The enormous amount of information was elegantly described in such an organized manner that readers in broad disciplines can easily overview the knowns and readily identify unknowns (Table 1) and gaps in knowledge as well as research (3). One of the important considerations articulated in this review article is that the mechanisms leading to the development and progression of NAFLD as well as the clinical manifestations of NAFLD are highly heterogeneous (3). This is in full agreement with information from a previous review article which specifically addressed, at the biopathological level, why some patients only develop bland steatosis while others either progress to/directly develop NASH or progress from NASH to cirrhosis (4). As wisely pointed out by the authors, current therapeutic strategies, especially combination therapies, are based on the assumption that all patients with the same histological appearance or stage of NAFLD arise from the same pathogenesis; undoubtedly, different individuals could have variable contributions from those convergent pathways which are dysregulated in the disease (3). This concept has indeed a strong physiopathological basis (4), and we wholeheartedly agree with their statement. The authors also suggested a possible data-driven approach to personalize therapeutic strategies based on response measures using hepatic gene expression or other -omics approaches (3). We feel there are some neglected areas to be further developed, namely sex differences and influences of sex hormones in NAFLD. This limitation, however, does not pertain to the article by Dr Friedman and colleagues but, rather, is attributable to the present literature in its whole, of which these authors’ review is certainly a faithful mirror.
Comment
Biologically relevant sex differences characterize female and male individuals, animals and cells; recognition of such differences is key to the progress of medicine and failure to accept sex-specific analysis in basic research will introduce bias into translational findings, clinical concepts, and drug development (5). Sex differences are widely accepted in various areas of clinical medicine, notably including cardiovascular and metabolic disorders, which are closely connected with NAFLD. Although full details cannot be discussed in this editorial due to word constraint, sex differences in NAFLD have been well demonstrated both in rodent models and in human disease. For example, when they are housed at standard housing (i.e., 20–23 °C), only male mice exhibit steatosis. However, thermoneutral housing (at 30–32 °C) reduces stress-induced corticosterone, augments proinflammatory immune responses, and will thus markedly exacerbate high fat diet-induced NAFLD pathogenesis, while diminishing sex difference in the development of steatosis (6).
In humans, the amount and distribution of body fat are under the control of endocrine signals (as shown by NAFLD being associated with Growth Hormone deficiency, hypothyroidism, and Polycystic Ovary Syndrome). The expression of myriads of genes in the liver, adipose tissue, and muscle, namely key-organs determining insulin resistance, significantly differ based on sex (7). Mitochondria, a key player in the pathogenesis of NASH at the cellular level, exhibit sexual dimorphism (8). Bile acid signaling and gut microbiota also express sex differences (9). Moreover, fructose consumption, a definite risk factor for the development of NAFLD, has been shown to be associated with activation of de novo lipogenesis more in women than in men (10). Collectively, these sex differences in the pathobiology of NAFLD and risk factors of NAFLD/NASH may account for some clinical and epidemiological differences of NAFLD in humans.
Despite these facts, research regarding sexual dimorphism in human NAFLD is probably lagging behind other areas of medicine. NAFLD is more prevalent in men and postmenopausal women compared to premenopausal women, partly due to an increased visceral fat accumulation (11). Women with NAFLD are approximately 10 years older than men (11); premenopausal status and synthetic hormone use have been associated with an increased histologic severity in NASH patients exposed at given levels of hepatic metabolic stress (12). The co-morbid conditions and risk factors for NAFLD may, in their turn, display sex differences. For example, as one study showed, NAFLD is specifically associated with an increased risk of colorectal adenomatous and hyperplastic polyps in men but not in women (13). Moreover, subclinical hypothyroidism was reportedly associated with a high risk of NAFLD in men rather than in women (14). In another study, serum uric acid was much more strongly associated with NAFLD in men than in women (15). Finally, it is also possible that the natural course of NAFLD is modulated by sex (5).
Conclusions and research agenda
NAFLD is a burgeoning metabolic epidemic with limited pharmacological therapeutic options. As commented above, the risk of development and progression of NAFLD is affected by sex and reproductive status via body fat distribution, insulin sensitivity, lipid homeostasis, immune response and cell reactivity to metabolic stress (4). Most experimental, clinical, epidemiological, and genetic studies in NAFLD, however, fail to consider such underlying biophysiology properly. On these grounds, we conclude that full exploration of sex differences in NAFLD and NASH is a major research gap which must be addressed at all levels from basic science to clinical trials. Such a characterization will advance our knowledge on the heterogeneity of NAFLD and help tailoring NAFLD care in the near future.
Acknowledgements
We would like to thank Ms. Jacqueline Mole for her accurate editing of English.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Italian Association for the Study of the Liver (AISF). AISF position paper on nonalcoholic fatty liver disease (NAFLD): Updates and future directions. Dig Liver Dis 2017;49:471-83. [Crossref] [PubMed]
- Lonardo A, Loria P, Argo C, et al. Perspectives on cellular dysfunction in nonalcoholic steatohepatitis: a case of ‘multiorganelle failure’? Proceedings of a virtual workshop on nonalcoholic steatohepatitis. Expert Rev Gastroenterol Hepatol 2011;5:135-9. [Crossref] [PubMed]
- Friedman SL, Neuschwander-Tetri BA, Rinella M, et al. Mechanisms of NAFLD development and therapeutic strategies. Nat Med 2018;24:908-22. [Crossref] [PubMed]
- Suzuki A, Diehl AM. Nonalcoholic Steatohepatitis. Annu Rev Med 2017;68:85-98. [Crossref] [PubMed]
- Ventura-Clapier R, Dworatzek E, Seeland U, et al. Sex in basic research: concepts in the cardiovascular field. Cardiovasc Res 2017;113:711-24. [Crossref] [PubMed]
- Giles DA, Moreno-Fernandez ME, Stankiewicz TE, et al. Thermoneutral housing exacerbates nonalcoholic fatty liver disease in mice and allows for sex-independent disease modeling. Nat Med 2017;23:829-38. [Crossref] [PubMed]
- Skubic C, Drakulić Ž, Rozman D. Personalized therapy when tackling nonalcoholic fatty liver disease: a focus on sex, genes, and drugs. Expert Opin Drug Metab Toxicol 2018;14:831-41. [Crossref] [PubMed]
- Ventura-Clapier R, Moulin M, Piquereau J, et al. Mitochondria: a central target for sex differences in pathologies. Clin Sci (Lond) 2017;131:803-22. [Crossref] [PubMed]
- Chiang JYL. Linking Sex Differences in Non-Alcoholic Fatty Liver Disease to Bile Acid Signaling, Gut Microbiota, and High Fat Diet. Am J Pathol 2017;187:1658-9. [Crossref] [PubMed]
- Low WS, Cornfield T, Charlton CA, et al. Sex Differences in Hepatic De Novo Lipogenesis with Acute Fructose Feeding. Nutrients 2018.10. [PubMed]
- Ballestri S, Nascimbeni F, Baldelli E, et al. NAFLD as a Sexual Dimorphic Disease: Role of Gender and Reproductive Status in the Development and Progression of Nonalcoholic Fatty Liver Disease and Inherent Cardiovascular Risk. Adv Ther 2017;34:1291-326. [Crossref] [PubMed]
- Yang JD, Abdelmalek MF, Guy CD, et al. Patient Sex, Reproductive Status, and Synthetic Hormone Use Associate With Histologic Severity of Nonalcoholic Steatohepatitis. Clin Gastroenterol Hepatol 2017;15:127-31.e2. [Crossref] [PubMed]
- Chen QF, Zhou XD, Sun YJ, et al. Sex-influenced association of non-alcoholic fatty liver disease with colorectal adenomatous and hyperplastic polyps. World J Gastroenterol 2017;23:5206-15. [Crossref] [PubMed]
- Lee J, Ha J, Jo K, et al. Male-specific association between subclinical hypothyroidism and the risk of non-alcoholic fatty liver disease estimated by hepatic steatosis index: Korea National Health and Nutrition Examination Survey 2013 to 2015. Sci Rep 2018;8:15145. [Crossref] [PubMed]
- Yu XL, Shu L, Shen XM, et al. Gender difference on the relationship between hyperuricemia and nonalcoholic fatty liver disease among Chinese: An observational study. Medicine (Baltimore) 2017;96:e8164. [Crossref] [PubMed]