
Trends and hotspots of prognostic factors for pancreatic ductal adenocarcinoma from 2013 to 2022
Pancreatic cancer, with its poor prognosis, holds the position of the 7th leading global cause of cancer deaths in both sexes in 2020 (1). In the United States, pancreatic cancer is the third leading cause of cancer-related deaths (2). Alarmingly, it was estimated that it would surpass colorectal cancer by 2040, ranking just after lung cancer as a primary cancer-related mortality cause (3). Pancreatic ductal adenocarcinoma (PDAC) is recognized as the most common type of pancreatic neoplastic disease (4). Apart from traditional surgical and chemotherapeutic methods, new developments in PDAC treatments, including genomic alterations, metabolic activities, tumor microenvironment, immunotherapy, and innovative clinical trial techniques, have been reported (5). Minimizing the health burden and enhancing disease prognosis necessitates the identification of certain factors and biomarkers to assist clinicians in accurately predicting the outcome for PDAC patients.
Joliat et al. (6) conducted a retrospective international study across six distinct centers between 2000 and 2017, involving 1,327 PDAC patients who received pancreatoduodenectomy. They enrolled four groups (entire cohort, pN+, pN1, and pN2), resulting in a median lymph node ratio (LNR) of 0.143 for the entire group and 0.214 for pN+ patients. Both the whole group and patients with pN+ showed an LNR threshold of 0.225, signifying a superior overall survival (OS) when the LNR was less than 0.225, as opposed to those with LNR of 0.225 or higher, according to the top Youden index indicative of OS exceeding 24 months. Patients in the pN1 group with LNR <0.225 and ≥0.225 demonstrated similar OS, while pN2 patients with LNR <0.225 had a better OS. Findings from the subgroup analysis of pN1 and pN2 indicated that LNR was able to stratify OS in pN2 patients. This result suggests that, according to the 8th edition of tumor-node-metastasis (TNM), LNR outperformed the pN stage in predicting survival likelihoods. Finally, they concluded that the LNR improved the forecasting of outcomes in patients with lymph node involvement and should be recommended as a regular supplement to the pN stage for more accurate patient prognosis prediction.
In addition to LNR, this study also identified the American Society of Anesthesiologists score, tumor grade, and adjuvant chemotherapy as independent indicators of OS. Joliat and his colleagues emphasized that neither the tumor’s size nor the status of the resection margin had any predictive impact on survival in the cohort. The study did not assess the continuous significance of LNR as a predictive factor in patients undergoing neoadjuvant treatment, a subject needing further exploration.
To analyze the trends and hotspots of prognostic factors for PDAC during the past 10 years, we sourced publications spanning 2013 to 2022 from the Web of Science Core Collection database and employed VOSviewer and Citespace to perform bibliometrics analysis. The retrieval strategy was as follows: ((TS = (prognostic factor)) OR TS = (prognosis)) AND TS = (Pancreatic ductal adenocarcinoma); Language = English; Document Type = (Articles OR Review Articles); and Time Range = January 1, 2013–December 31, 2022.
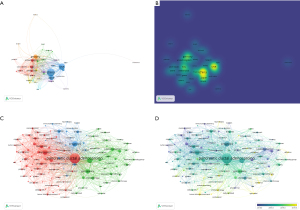
We retrieved 4,535 publications from 81 countries. In Figure 1A, 44 countries were divided into eight clusters when the minimum number of documents of a country was five. A density visualization map of the co-authorship of countries was shown in Figure 1B. Diverse colors symbolized the frequency of co-authorship of countries, with yellow denoting the most frequent. China, the United States, and Germany have relatively close cooperative relations. VOSviewer was utilized to analyze the co-occurrence of keywords, creating network and overlay visualization maps. The 119 keywords were divided into three clusters when the minimum number of occurrences per keyword was 50 (Figure 1C). The top five most frequent keywords were “pancreatic ductal adenocarcinoma” [3,904], “overall survival” [1,191], “prognosis” [1,029], “expression” [885], and “gemcitabine” [737]. The line between “pancreatic ductal adenocarcinoma” and “overall survival” was the thickest, indicating that OS has been an important measurement for prognostic factors of PDAC in the past 10 years. As shown in Figure 1D, “folfirinox”, “liquid biopsy”, and “open-label” were the keywords that have received more attention since 2020. We used Citespace to analyze the keywords with the strongest citation bursts regarding the prognosis of PDAC, and the results are demonstrated in Figure 2. The keywords “k-ras” (13.81) and “endothelial growth factor” (10.61) showed the strongest bursts from 2013 to 2022, and the keywords “liquid biopsy” and “targeted therapy” began to burst in 2020 and continued until 2022.
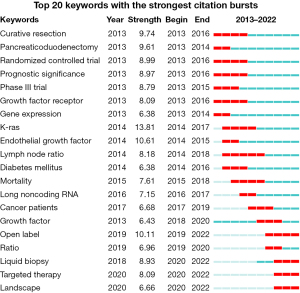
Overall, China had the most publications on the prognosis of the PDAC. The escalating burden of pancreatic cancer in China could be the reason. It was reported that the burden associated with pancreatic cancer has been increasing in China from 2005 to 2020. A total of 100,427 pancreatic cancer deaths and 2,166,355 pancreatic cancer-related years of life lost were estimated in China in 2020 (7). Additionally, the United States maintained comparatively tight collaborative ties with China, Japan, Germany, and other countries. The rising mortality of pancreatic cancer in the United States, coupled with its global medical dominance, were significant factors. In this study, we found the LNR was a hotspot from 2014 to 2018. Some studies, as mentioned by Joliat et al. in their study, have highlighted the important role of LNR in the staging and prognosis of pancreatic cancer (8,9). Following the creation of the pN2 in the 8th edition of the TNM classification, which has been in use since 2018, it becomes significant to explore the adaptability of LNR in the latest staging version. This is exactly the outstanding contribution provided by Joliat and his colleagues. Concurrently, the “k-ras” and “endothelial growth factor” emerged as focal points during that era. These hotspots were continually changing. Lately, the fields of “liquid biopsy” and “targeted therapy” have emerged as prominent research areas. The application of liquid biopsy for diagnosis, treatment, and prognosis of PDAC has undergone a thorough investigation (10,11). Many studies (12,13) have intensely focused on targeted therapy in PDAC. The critical role of targeted therapy in improving the prognosis for PDAC is well acknowledged, with further studies in this field being emphasized. Moreover, various hotspots have experienced rapid advancements and integrations.
In conclusion, although surgery and chemotherapy continue as the main treatments of PDAC, the targeted therapy represents an innovative and robust approach. Despite ongoing advancements in treatment, the significant worldwide influence of PDAC is intensifying, requiring continuous efforts to improve the prognosis of the disease.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Hepatobiliary Surgery and Nutrition. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://hbsn.amegroups.com/article/view/10.21037/hbsn-23-667/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. [Crossref] [PubMed]
- Siegel RL, Miller KD, Wagle NS, et al. Cancer statistics, 2023. CA Cancer J Clin 2023;73:17-48. [Crossref] [PubMed]
- Rahib L, Wehner MR, Matrisian LM, et al. Estimated Projection of US Cancer Incidence and Death to 2040. JAMA Netw Open 2021;4:e214708. [Crossref] [PubMed]
- Kleeff J, Korc M, Apte M, et al. Pancreatic cancer. Nat Rev Dis Primers 2016;2:16022. [Crossref] [PubMed]
- Halbrook CJ, Lyssiotis CA, Pasca di Magliano M, et al. Pancreatic cancer: Advances and challenges. Cell 2023;186:1729-54. [Crossref] [PubMed]
- Joliat GR, Labgaa I, Sulzer J, et al. International assessment and validation of the prognostic role of lymph node ratio in patients with resected pancreatic head ductal adenocarcinoma. Hepatobiliary Surg Nutr 2022;11:822-33. [Crossref] [PubMed]
- Xu Y, Liu W, Long Z, et al. Mortality and years of life lost due to pancreatic cancer in China, its provinces, urban and rural areas from 2005 to 2020: results from the national mortality surveillance system. BMC Cancer 2023;23:893. [Crossref] [PubMed]
- Pomianowska E, Westgaard A, Mathisen Ø, et al. Prognostic relevance of number and ratio of metastatic lymph nodes in resected pancreatic, ampullary, and distal bile duct carcinomas. Ann Surg Oncol 2013;20:233-41. [Crossref] [PubMed]
- Tol JA, Brosens LA, van Dieren S, et al. Impact of lymph node ratio on survival in patients with pancreatic and periampullary cancer. Br J Surg 2015;102:237-45. [Crossref] [PubMed]
- Vidal L, Pando E, Blanco L, et al. Liquid biopsy after resection of pancreatic adenocarcinoma and its relation to oncological outcomes. Systematic review and meta-analysis. Cancer Treat Rev 2023;120:102604. [Crossref] [PubMed]
- Watanabe F, Suzuki K, Noda H, et al. Liquid biopsy leads to a paradigm shift in the treatment of pancreatic cancer. World J Gastroenterol 2022;28:6478-96. [Crossref] [PubMed]
- Qian Y, Gong Y, Fan Z, et al. Molecular alterations and targeted therapy in pancreatic ductal adenocarcinoma. J Hematol Oncol 2020;13:130. [Crossref] [PubMed]
- Huffman BM, Ellis H, Jordan AC, et al. Emerging Role of Targeted Therapy in Metastatic Pancreatic Adenocarcinoma. Cancers (Basel) 2022;14:6223. [Crossref] [PubMed]


