A “reappearance” of gallbladder in a liver transplant recipient
In liver transplantation graft cholecystectomy is performed routinely. Bile leaks have an incidence of 2–25% following liver transplantation. Most bile leaks are diagnosed within 30 days and rarely after 3 months. In this article, we describe a case of biloma with stones “neo-gallbladder” 5 years after transplantation. The initial clinical presentation was pancreatitis and “acute cholecystitis”. The patient underwent surgical exploration and a Roux-en-Y hepaticojejunostomy was performed.
A 60 years old man with end stage liver disease secondary to alcoholic cirrhosis received a liver transplantation from a deceased donor. The postoperative period was unremarkable and the patient was discharged 14 days after the intervention. The patient was follow up until 2 months after the transplantation then he lost to follow up due to resumption of alcohol intake. Liver function test and the follow up liver US were normal during the 2-month follow up.
Five years later, he presented to the emergency department with right upper quadrant associated with fever and vomiting. On clinical examination, there was tenderness in the right hypochondrium. He was found to have abnormal liver function test with elevated gamma-glutamyltransferase (GGT), alkaline phosphatase (alk phos), and total bilirubin (TBIL).
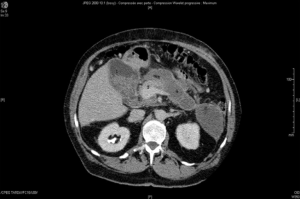
CT-scan was done which showed signs of acute pancreatitis classified as (Balthazar radiologic score: E) associated with common bile duct and intra hepatic duct dilatation. The CT scan showed as well impacted stones in the common bile duct and apparently gallbladder stones (Figure 1). There were no signs of portal vein thrombosis and hepatic artery thrombosis. The patient was admitted to the ICU for severe sepsis. Decision was taken to do surgical exploration.
A right subcostal incision was performed. The Surgical exploration of the abdomen revealed a bile collection with multiple stones content. After evacuation of the collection and removal of the stones, we found bile leak from the biliary anastomosis between graft and donor bile duct. Intraoperative choledocoscopy was performed to ensure complete clearance of the donor and recipient biliary tracts from the stones. The bile duct of the LT recipient was then closed, and a Roux-en-Y anastomosis was performed.
Biliary tract complications are the most common complications after liver transplantation. These complications include strictures, leaks, stones and recurrence of biliary disease like primary biliary cirrhosis and primary sclerosing cholangitis. bile leak is considered to be the most common among these complication. Bile leaks have an incidence of around 2–25% following liver transplantation (1) and may arise from the anastomosis, cystic duct remnant, failure to recognize anomalies of the biliary tree, T-tube tract, or from the cut surface of the liver (in the case of living donor LT or partial liver grafts).
Most bile leaks are diagnosed within 30 days and rarely after 3 months (2), clinical presentation is variable, ranging from asymptomatic drainage of biliary fluid to life threatening conditions such as a biliary sepsis requiring relaparotomy.
A biloma may develop after bile leak. The biloma is a bile collection outside the biliary tree which can be extra or intra hepatic, encapsulated or not. The median time for the diagnosis of bilomas is usually 1–2 weeks following bile duct injury (or bile leak). We have found a case report in the literature which reported a biloma 5 years after bile duct injury during cholecystectomy. In another report diagnosis was done nine years after the initial event (3).
Biliary filling defects occur in approximately 5–6% of patients after LT and may be referred to gallstones, sludge, debris, blood clots, and casts (4). However, about 70% of such defects are caused by biliary stones (4). Patients develop this complication at a median period of 1,500 days after transplantation (5). The clinical presentation of patients with common bile duct stones vary from asymptomatic cholestasis, to abdominal pain, or recurrent attacks of cholangitis or pancreatitis. With elevated liver enzymes one must exclude vascular insult to the liver like portal vein thrombosis and hepatic artery thrombosis. Management is similar to the non-transplant patients and is based on endoscopic retrograde cholangiopancreatography (ERCP) with a high rate (up to 90%) of successful endoscopic stone extraction (4). Moreover, additional endoscopic dilatation and stenting may be necessary to treat coexistent biliary strictures associated in 40% of post-LT biliary tract calculi (4). After successful endoscopic management, there is approximately a 17% recurrence rate within a median of 6 months (6). If endoscopic therapy fails, surgical extraction, conversion to Roux-en-Y choledochojejunostomy, or retransplantation, may be required.
Our patient developed a biliary complication 5 years after transplantation. His initial presentation was sepsis and acute pancreatitis. The appearance of the collection in the gallbladder bed in the CT scan with the stones contents resemble the appearance of a normal gallbladder. In conclusion there are four factors which predict the occurrence of biliary complications after liver transplantation: male sex, cyclosporine therapy, acute cellular rejection and hepatic artery thrombosis (7). In our case only the gender was a risk factor. After 5 years, our patient is still alive and has not developed any further complication.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this article and any accompanying images.
References
- Ayoub WS, Esquivel CO, Martin P. Biliary complications following liver transplantation. Dig Dis Sci 2010;55:1540-6. [Crossref] [PubMed]
- Khuroo MS, Al Ashgar H, Khuroo NS, et al. Biliary disease after liver transplantation: the experience of the King Faisal Specialist Hospital and Research Center, Riyadh. J Gastroenterol Hepatol 2005;20:217-28. [Crossref] [PubMed]
- Kannan U, Parshad R, Regmi SK. An unusual presentation of biloma five years following cholecystectomy: a case report. Cases J 2009;2:8048. [PubMed]
- Porrett PM, Hsu J, Shaked A. Late surgical complications following liver transplantation. Liver Transpl 2009;15 Suppl 2:S12-8. [Crossref] [PubMed]
- Moser MA, Wall WJ. Management of biliary problems after liver transplantation. Liver Transpl 2001;7:S46-52. [Crossref] [PubMed]
- Balderramo D, Navasa M, Cardenas A. Current management of biliary complications after liver transplantation: emphasis on endoscopic therapy. Gastroenterol Hepatol 2011;34:107-15. [Crossref] [PubMed]
- Donovan J. Nonsurgical management of biliary tract disease after liver transplantation. Gastroenterol Clin North Am 1993;22:317-36. [PubMed]


