Gallbladder carcinoma post gallbladder-preserving cholecystolithotomy: a case report
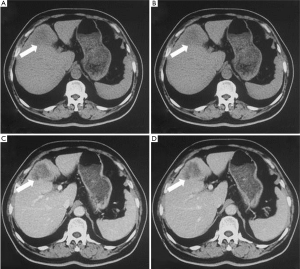
A 76-year-old male with a ten-year history of cholelithiasis with intermittent right upper quadrant pain presented at clinic in March, 2010. Cholecystolithotomy via choledochoscopy was performed 5 years ago, 4 months after which, recurrence of the stones was confirmed. The irregularly episodic pain with distention developed 2 years ago. Levels of carcinoembryonic antigen (CEA 61.22 ng/mL) and carbohydrate antigen 125 (CA125 162.9 U/mL) were increased, whereas alfa-fetal protein (AFP) and carbohydrate antigen 19-9 (CA19-9) were normal. Ultrasound examination found an irregular and ill-demarcated hypoechoic lesion (6.2 cm × 3.4 cm) and multiple hyperechoic spots with acoustic shadow within the gallbladder. Contrast-enhanced computed tomography (CECT) detected a low-density mass embedded within the enlarged and distorted gallbladder with irregular enhancement and adjacent liver involvement (Figure 1). In the laparotomy, a firm whitish lesion about 2 cm × 3 cm was found at the fundus of the gallbladder, which was imbedded in the previous incision of the gallbladder. Malignancy was confirmed by frozen section, and a radical resection for gallbladder carcinoma with quadrate lobectomy was performed.
Gross pathological examination showed a semi-firm tumor (5.5 cm × 3 cm × 2 cm) residing at the fundus of the gallbladder, with transmural invasion into the adjoining liver. Hematoxylin and eosin (H&E) staining showed poor to moderately differentiated adenocarcinoma, involving muscular, serosal. Immunohistochemistry was positive for CEA and cytokeratin (CK19, CK7, CK8), justifying the origination from the epithelium of the gallbladder.
Discussion
Cholelithiasis has been regarded as the best known and most important risk factor for gallbladder carcinoma, supporting by that gallstones are found in 65-90% of patients with gallbladder cancer (1). Relative risk for gallbladder neoplasia could be four to five times higher in patients with gallstones than in acalculous individuals (2). This has also been justified by the findings of epithelial dysplasia, atypical hyperplasia, and carcinoma in situ (seen in 83%, 13.5%, and 3.5% of patients, respectively), in gallbladders removed for treatment of gallstones (3). Cholecystectomy has been worshipped as the gold standard for the treatment of cholelithiasis since its coming into the history. However, it has been in hot debates in recent years, that whether the gallbladder should always be executed irrespective of its physiological role and the resulting alteration on the quality of life after its removal. Gallbladder-preserving procedure, serving as an alternative approach for the treatment of cholelithiasis, has witnessed its evolution over the past two decades, from minimally invasive surgery to cholecystolithotomy via choledochoscopy. High rates for success have been showcased in most studies and reports (4), in China particularly, among which major concerns have been focused on stone re-growth within the retained gallbladder after stones are removed by choledochoscopy, while cases of gallbladder carcinoma after gallbladder-preserving therapy have rarely been documented (5). Our case has demonstrated a typical picture of progression from silent gallstones to clinical cholelithiasis to gallbladder carcinoma eventually. Surgeons especially those in the developing countries should take this in mind while further pursuit cholecystolithotomy.
Acknowledgements
We thank Tianyi Chi, Haitao Zhao, Yiyao Xu, Haifeng Xu, Huayu Yang for helping collecting clinical images and data. National Natural Science Foundation of China (30901453) supporting in the writing of the report.
Disclosure: The authors declare no potential conflicts of interest.
References
- Misra S, Chaturvedi A, Misra NC, et al. Carcinoma of the gallbladder. Lancet Oncol 2003;4:167-76. [PubMed]
- Lowenfels AB, Maisonneuve P, Boyle P, et al. Epidemiology of gallbladder cancer. Hepatogastroenterology 1999;46:1529-32. [PubMed]
- Albores-Saavedra J, Alcántra-Vazquez A, Cruz-Ortiz H, et al. The precursor lesions of invasive gallbladder carcinoma:hyperplasia, atypical hyperplasia and carcinoma in situ. Cancer 1980;45:919-27. [PubMed]
- Liu JS, Li JZ, Zhao QK, et al. The analysis of follow-up results of 612 cases of cholecystolithiasis treated with the minimal invasive operation with gallbladder preserved via choledochoscopy. Chin J Surg 2009;47:279-81. [PubMed]
- So CB, Gibney RG, Scudamore CH. Carcinoma of the gallbladder: a risk associated with gallbladder preserving treatments for cholelithiasis. Radiology 1990;174:127-30. [PubMed]


