Racial disparities in treatment and survival of patients with hepatocellular carcinoma in the United States
Introduction
Hepatocellular carcinoma (HCC) constitutes 4.6% of all new cancer cases and represents the fifth leading cause of cancer-related death worldwide (1-3). Although HCC is less common in the United States (US) compared with Africa and Eastern Asia, the incidence and mortality associated with HCC have been steadily increasing in the US over the past two decades (4-7). Furthermore, HCC is of interest in that it disproportionally affects all US racial/ethnic minority populations (8-10). In particular, the incidence of HCC is over two fold higher among Asian- and African-Americans compared with Caucasian patients in the US (8-10). Of note, recent studies have reported HCC-related mortality to have increased by 2.1%, 2.4% and 1.3% per year among white, black and Hispanic patients, respectively, between 2000 and 2010, but decreased by 1.6% per year among Asian patients (5).
Accounting for this disparity is likely multifaceted and may be due to social, biological and financial factors. For example, socioeconomic and insurance status may limit access to appropriate preventive and surveillance measures resulting in a higher incidence among older, minority and uninsured patients (8-10). Similarly, as complex surgical resection is the mainstay for treatment, patients may have to travel long distances to receive care at large, specialized centers. A recent study demonstrated that although only 40% of patients with HCC received surgical treatment, older patients as well as racial minorities had lower rates for surgery after controlling for disease and comorbid illnesses (9,11,12). Further, as demonstrated by Luo et al. cultural beliefs and attitudes as well as patient-physician communication can be critical to appropriate treatment decision-making among minority patients with cancer (11). In contrast, other reports have attributed this disparity to disease biology demonstrating that African Americans may present with more advanced, metastatic disease which may therefore be less amenable to cure (9). Although widely recognized and reported on for other cancers, data focusing on ethnicity-based clinical presentation, management, and survival among HCC patients are still limited. In addition, the reasons that drive racial differences in incidence and survival among these patients remain poorly understood. Given this, the present study aimed to examine racial differences in treatment modality and survival among patients presenting with HCC in the US.
Methods
Data sources and study population
Patients presenting with HCC were identified using the Surveillance Epidemiology, and End Results (SEER) database from 1998 to 2012 (13). Maintained by the National Cancer Institute, the SEER registry database collects patient and disease specific data from local and regional cancer registries and is a representative sample of 28% of the US population. Standard patient demographic and clinicopathologic data including gender, age at diagnosis, year of diagnosis, tumor size, stage at diagnosis, alpha fetoprotein (AFP) levels, presence of cirrhosis, and tumor grade of differentiation were collected.
Patients with HCC were identified using International Classification of Diseases for Oncology, Third Edition (ICD-O-3) topography and morphology codes. Specifically “primary site” code “C220” and “histologic type” codes “8170,” “8172,” “8173,” “8174,” and “8175” were used to select for patients. A confirmed diagnosis of HCC was defined as either a positive microscopic result, laboratory test/marker, direct visualization, or positive radiology and imaging. Patients with histology codes other than those representing HCC and patients with HCC diagnosed upon autopsy were excluded from the analysis. Similarly, records with missing information for age, and race as well as patients younger than 18 years were excluded. Further, due to marked differences in epidemiology and prognosis, patients presenting with fibrolamellar carcinoma was also excluded from the study cohort (14,15).
Patient race was categorized as white, black, Asian (Asian/Pacific Islander), and native American (American Indian/Alaska native) based on SEER coding scheme (13). Type of treatment was determined using SEER site-specific surgery of primary site codes and radiation therapy codes. Surgical management was defined as either a liver resection and/or a liver transplant while ablation was defined as heat-radio-frequency ablation, photodynamic therapy, electrocautery, fulguration, cryosurgery, laser, or alcohol and acetic acid ablation and considered as non-surgical treatment. Patients were categorized into treatment groups based on the treatment received for primary disease. In the instance where a patient received multiple types of treatments for the same disease episode, they were categorized based on highest level of treatment. For example, if a patient underwent both radiation and surgery, they were categorized as having undergone surgery for their primary disease. Stage at diagnosis was defined as either localized, regional disease, distant disease, or unstaged. Tumor grade was classified using SEER grading and differentiation codes whereby grade I represented well-differentiated disease, grade II; moderately differentiated, grade III; poor differentiated and grade IV representing undifferentiated disease. For ease of analysis, grade was categorized as a binary variable combing grades I and II into a single category and grades III and IV into another. Cirrhosis was defined using the SEER site-specific fibrosis score, classifying patients presenting with a fibrosis score of ≥5 as cirrhotic. Vital status was recorded for all cases, and the date of latest follow-up was December 31, 2012.
Statistical analysis
Descriptive statistics were reported as medians with interquartile range (IQR) for continuous variables and as whole numbers and percentages for categorical variables. Descriptive statistics for discrete variables were compared using the Chi square and Fisher’s exact test, where appropriate. The Kruskal-Wallis test was used to compare continuous variables. Multivariable logistic regression analysis was performed to identify factors determining treatment modality for HCC (surgical vs. non-surgical therapy). The Kaplan-Meier method was used to assess stage-adjusted and treatment-adjusted survival. A multivariable Cox proportional hazards models was built to determine factors predictive of survival. All variables of clinical importance were included in multivariable analysis. Since AFP and cirrhosis are important clinical factors for treatment and survival of HCC, only patients with information pertaining to AFP and severity of cirrhosis were included in multivariable analysis (patients diagnosed after 2004). The prognostic power of covariates was expressed as HRs with 95% confidence intervals. Statistical significance was defined as P<0.05 (two-sided). All analyses were performed using STATA version 12.0 (StataCorp LP, College Station, TX, USA).
Results
Racial disparities in demographic and tumor features
A total of 58,186 patients with HCC were identified and met inclusion criteria. The median age of the cohort was 62 years (IQR, 55-73 years) with a majority of patients being male (n=44,339, 76.2%). Over two-thirds of patients were white (n=39,223, 67.4%) while 13.1% (n=7,620) of the cohort were black, 1.2% (n=678) native American and 18.3% (n=10,665) Asian. The median tumor size was 5.0 cm (IQR, 3.0-8.0) with approximately half of all patients presenting with localized disease (n=27,207, 46.8%) and 24.8% (n=5,600) of patients presenting with high grade (grade III or IV) lesions. Data pertaining to serum AFP and cirrhosis were available for 32,109 and 10,263 patients respectively. Among these patients, 23.3% (n=7,484) presented with elevated AFP levels at diagnosis while a majority of patients had concomitant cirrhosis (n=8,117, 79.1%) (Table 1).
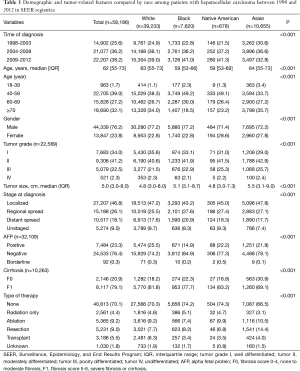
Full table
Marked differences were noted in baseline demographic and disease characteristics by race (Table 1). For example, white and Asian patients were older compared with black and native American patients (white vs. black vs. native American vs. Asian: median age: 63 years, IQR, 55-73 vs. 59 years, IQR, 53-66 vs. 59 years, IQR, 53-69 vs. 64 years, IQR, 55-73, all P<0.001). Similarly, Asian and Native American patients were more likely to be female vs. white and black patients (white vs. black vs. native American vs. Asian: 22.8% vs. 22.8% vs. 28.6% vs. 27.8%, all P<0.001). On average, Asian patients presented with larger tumors compared with other racial groups (white vs. black vs. native American vs. Asian: median tumor size: 4.8 cm, IQR, 3.0-8.0 vs. 5.1 cm, IQR, 3.1-8.7 cm vs. 4.8 cm, IQR, 3.0-7.3, vs. 5.5 cm, IQR, 3.1-9.0, all P<0.05) and were more likely to present with localized disease (white vs. black vs. native American vs. Asian: 47.2% vs. 43.2% vs. 45.0% vs. 47.8%, all P<0.05). Compared with other racial groups, Asian patients were proportionally less likely to present with cirrhosis at diagnosis (white vs. black vs. native American vs. Asian: 81.8% vs. 77.7% vs. 83.2% vs. 69.1%, all P<0.05). While an elevated AFP was detected in over a fifth of patients, black patients were the least likely to present with an elevated AFP at diagnosis (white vs. black vs. native American vs. Asian: 25.5% vs. 14.9% vs. 22.2% vs. 21.8%, all P<0.001).
Racial disparities in treatment
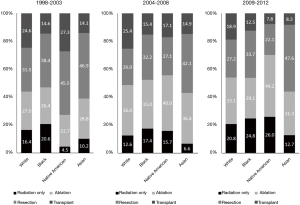
Among all patients, less than 30% of patients received any type of treatment for HCC (n=12,789, 29.5%), with Asian patients more likely to receive treatment for HCC compared with other racial groups (white vs. black vs. native American vs. Asian: 29.2% vs. 25.2% vs. 27.6% vs. 34.4%, all P<0.001). In addition, differences in the type of treatment were also noted by race among patients that received any form of treatment for HCC. For example, Asian patients were proportionally more likely to be treated surgically either with resection or a liver transplant compared with other racial groups (white vs. black vs. Native American vs. Asian: 14.3% vs. 11.8% vs. 10.1% vs. 19.4, all P<0.001, Table 1). Similar patterns in treatment were also noted throughout the time period of the study among the different racial groups (Figure 1). Of note, among patients that received any form of treatment, white patients were the racial group most likely to receive a liver transplant compared with other racial groups. This pattern was consistent throughout the study period. The proportion of patients that underwent ablation of a lesion increased throughout the study time period with a similar trend observed among all racial groups. Specifically among patients that received any form of treatment 18.0% (n=43) patients received an ablation for their lesion in 1998 compared to 36.2% (n=398) in 2004 and 33.4% (n=563) in 2012, with Native American patients proportionally more likely to be managed via ablation compared to all other racial groups (Figure 1).
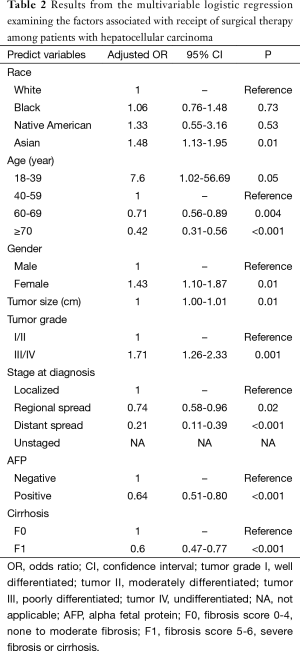
To assess the factors associated with receiving surgical treatment (liver resection and/or transplant) for HCC, multivariable analysis was performed controlling for patient demographics and disease characteristics (Table 2). In particular, increasing age was associated with decreased odds of undergoing surgery (60-69 years: OR: 0.71, 95% CI, 0.56-0.89, P=0.004; ≥70 years: OR: 0.42, 95% CI, 0.31-0.56, P<0.001) while female patients demonstrated greater odds to undergo surgery compared with male patients (OR: 1.43, 95% CI, 1.10-1.87, P=0.01). Interestingly, while white, black and Native American patients were just as likely to undergo surgery, Asian patients demonstrated a 48% greater odds of undergoing surgery (OR: 1.48, 95% CI, 1.13-1.95, P=0.01). Similarly, patients with higher tumor grade demonstrated greater odds of undergoing surgery (grade III/IV: OR: 1.71, 95% CI, 1.26-2.33) while patients with metastatic disease (regional metastasis: OR: 0.74, 95% CI 0.58-0.96, P=0.02; distant metastasis: OR: 0.21, 95% CI, 0.11-0.39, P<0.001) as well as patients with elevated AFP (OR: 0.64, 95% CI, 0.51-0.80, P<0.001) or cirrhosis at diagnosis (OR: 0.60, 95% CI, 0.47-0.77, P<0.001) demonstrated decreased odds of undergoing surgery (Table 2).
Full table
Racial disparities in overall survival (OS)
Median OS for the entire cohort was 11 months while 1-, 3-, and 5-year survival were 47.8%, 25.5%, and 18.1%, respectively. Racial differences were noted in OS. Asian patients demonstrated the highest OS of 15 months compared with white, black and native American patients who had an OS of 11 months, 9 months and 12 months, respectively (all P<0.05). Similarly, 5-year survival was highest among Asian patients compared with other racial groups (white vs. black vs. native American vs. Asian: 17.5% vs. 12.4% vs. 17.7% vs. 23.8%, all P<0.001). These racial differences in survival were also noted after stratifying by disease stage (Figure 2A,B). Specifically, among patients with localized disease, 1-, 3- and 5-year OS was highest among Asian patients (white: 62.8%, 37.1%, 27.2% vs. black: 60.5%, 31.8%, 21.2% vs. native American: 63.5%, 37.8%, 27.2% vs. Asian: 71.4%, 47.5%, 36.1%, all P<0.05). In contrast, patients with metastatic disease, 1-, 3-, and 5-year OS was lowest among black patients (white: 30.5%, 11.6%, 7.5% vs. black: 25.7%, 8.7%, 4.5% vs. native American: 30.6%, 13.7%, 8.6% vs. Asian: 34.0%, 15.7%, 10.8%, all P<0.05).
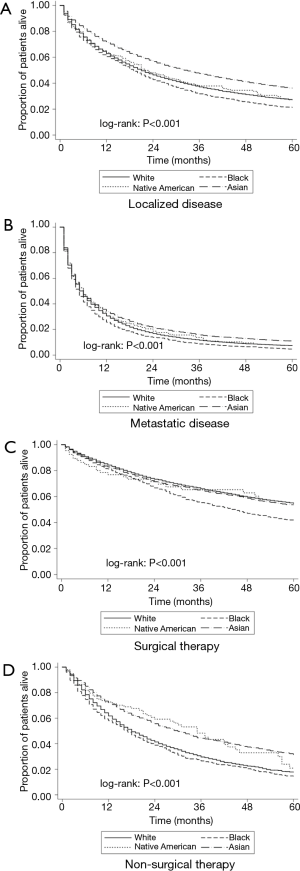
A similar trend in survival was noted among racial groups when stratified by treatment. Among patients who underwent surgery, black patients had the worst prognosis compared with other races, while a similar survival was noted among white and Asian patients (1-, 3- and 5- years OS: white 84.3%, 66.0%, 54.7% vs. black: 81.3%, 55.3%, 40.9% vs. native American: 76.8%, 65.3%, 57.8% vs. Asian: 82.8%, 64.6%, 53.5%, P<0.001, Figure 2C). For patients who were managed non-surgically, Asian patients demonstrated the best prognosis while black patients demonstrated the lowest survival. Specifically, the 1-, 3-, and 5-year OS of Asian patients who underwent non-surgical therapy were 72.2%, 44.3%, and 31.3%, vs. 61.8%, 29.6%, and 17.8% among white patients (P<0.001), and 58.0%, 26.5%, and 14.5% among black patients (P<0.001, Figure 2D).
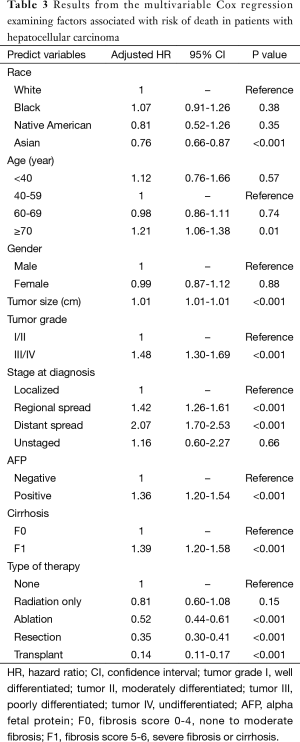
On multivariable analysis after adjusting for patient and disease characteristics, Asian patients demonstrated the lowest risk of death compared with white patients (HR: 0.76, 95% CI, 0.66-0.87, P<0.001). In addition, no differences in survival were noted among white, black and native American patients (all P>0.05, Table 3). Other patient and disease characteristics associated with a poor prognosis included age ≥70 years (HR: 1.21, 95% CI, 1.06-1.38, P=0.01), tumor size (HR: 1.01, 95% CI, 1.01-1.01, P<0.001), a higher tumor grade (grade III/IV: HR: 1.48, 95% CI, 1.30-1.69, P<0.001), metastatic disease (regional metastasis: HR: 1.42, 95% CI, 1.26-1.61, P<0.001; distant metastasis: HR: 2.07, 95% CI, 1.70-2.53, P<0.001), elevated AFP levels (HR: 1.36, 95% CI, 1.20-1.54, P<0.001) and cirrhosis at presentation (HR: 1.39, 95% CI, 1.20-1.58, P<0.001). Furthermore, compared to patients that did not receive any treatment, patients that received a liver transplantation demonstrated the lowest risk of death (HR: 0.14, 95% CI, 0.11-0.17, P<0.001) followed by patients that underwent a surgical resection (HR: 0.35, 95% CI, 0.30-0.41, P<0.01) or ablation (HR: 0.52, 95% CI, 0.44-0.61, P<0.001). Of note, radiation alone did not decrease the risk of death among patients with HCC (HR: 0.81, 95% CI, 0.60-1.08, P=0.15, Table 3).
Full table
Discussion
HCC represents the third leading cause of cancer-related death worldwide (1,2). Although HCC is less frequently encountered in the US compared with Africa and Eastern Asia, recent years have seen a steady increase in the incidence and mortality of HCC in the US (4-6). Of note, recent studies have suggested that racial differences exist among patients with HCC with regard to incidence and mortality (7,8,10,16). Using a nationally representative cohort of patients with HCC, the present study characterized racial differences in survival and treatment choices among patients. To our knowledge, this is the first study to report racial disparities among patients undergoing medical or surgical treatment for HCC in the US over a span of over 20 years. In particular, we noted significant differences in presentation by race with black patients being more likely to present with metastatic disease, while Asian patients were the least likely to present with concomitant liver cirrhosis. After accounting for patient and disease characteristics, Asian patients were most likely to undergo a liver resection, with liver transplantation being more common among white patients. Furthermore, Asian patients demonstrated a 24% lower risk of mortality compared with white patients.
While racial disparities have been well-documented for multiple cancers, less is known regarding racial disparities for HCC. In the current study of over 58,000 patients, we noted racial differences not only in the treatment of HCC but also significant differences in disease presentation by race. These data suggest that etiological factors as well as socio-demographic factors may play important roles in explaining observed disparities. For example, previous reports have demonstrated that Asian patients tend to present with HCC that develops in a non-cirrhotic liver due to chronic hepatitis B virus infection and therefore may be more amenable to surgery (8,17,18). Supporting this notion, the current study noted that Asian patients were the racial group least likely to present with underlying cirrhosis. In addition, Asian patients also had a 48% greater odds of undergoing surgical resection for HCC compared with white patients. In contrast, the current study noted that black patients were proportionally more likely to present at a later stage/with metastatic disease. While recent reports suggest genetic variations in tumor biology and pathogenesis among patients, differences noted in our study also serve to highlight disparities in access to adequate screening and preventive measures. In their recent report, Davila et al. reported significantly lower rates of screening and surveillance for HCC among black and Hispanic patients while Asian patients, patients of a higher median household income and patients with a higher level of education were almost two-fold more likely to receive HCC surveillance (19). These data are consistent with findings from the current study that noted a large variation in the stage of disease among patients from different racial groups. Taken together, the data suggest that while potentially efficacious interventions in the form early detection via the use of surveillance ultrasounds and targeted, more frequent screening programs for HCC among high-risk groups are available, access to such parameters are limited and can vary by racial/ethnic groups. In turn, these socio-demographic inequalities may result in disparities in treatment and subsequent survival.
In addition to variations in screening, differences in treatment choices may also be affected by patient preferences, socio-demographic differences and access to care (8,10). The decision-making process for treatment among HCC patients is complicated, especially given the advent of novel therapies and the increasing use of a multidisciplinary approach (20). With patients increasingly involved in the selection of their treatment, cultural attitudes and communication between patient and provider can significantly affect choice of treatment (9,11). For example, Lin et al. reported higher levels of medical mistrust and fatalism among certain minority patients undergoing cancer surgery (21). Coupled together, medical mistrust and fatalism have been associated with decreased follow-ups, lower adherence to treatment plans as well as higher rates of refusal for potentially curative surgery. Mathur et al. noted that even among patients presenting with early stage HCC, only 40% of patients received surgery with markedly lower rates among minority, uninsured and elderly patients (8). Similarly Zak and colleagues reported that minority serving hospitals were less likely to offer surgical treatment after accounting for disease severity (9). In the current study, we similarly noted that differences in receipt of treatment among different patient cohorts. For example, Asian patients were proportionally more likely to be treated surgically either with resection or a liver transplant compared with other racial groups (white vs. black vs. native American vs. Asian: 14.3% vs. 11.8% vs. 10.1% vs. 19.4, P<0.001) (Figure 1). In turn, perhaps not surprisingly, these differences in disease presentation and receipt of treatment translated into disparate race based survival outcomes. Specifically, Asian patients had an overall better survival compared with other racial groups even after controlling for available factors in the dataset. In contrast, black patients had the worst survival. Moving forward, policies will need to be developed that specifically target racial disparities such as implementing culturally sensitive screening and preventive programs, as well as increasing awareness and education regarding disparities in HCC outcomes among health care providers.
The current study had several limitations. There may have been some discordance in the reporting of race between self-reported and registry records, which may have possibly impacted the results (12). However, any reporting bias would likely be random and not affect the main findings of the study. Further, the lack of granular information pertaining to tumor specific data including the Barcelona clinic liver cancer (BCLC) staging system and other clinically relevant risk factors such as preexisting hepatitis infections limited our ability to explain differences in disease presentation. Similarly, a lack of data pertaining to the use of trans arterial chemo-embolization, systemic chemotherapy or laparoscopic ablation in the SEER-dataset may have led to an underestimation of certain treatment received. Finally, details pertaining to socioeconomic and insurance status, which may play an important role in driving differences in treatment and survival, were not available in the SEER-database and therefore could not be accounted for.
Conclusions
In conclusion, treatment and mortality for HCC in the US vary substantially by race. After adjusting for several disease factors, Asian patients were more likely to undergo potentially curative therapy such as resection and transplantation and, in turn, Asian patients with HCC had the best OS compared with other racial groups. In contrast, black patients were less likely to receive treatment and demonstrated a worse prognosis compared with other racial groups. Future policies should focus of improving access to care/treatment among minority groups, which is a prerequisite to improving outcomes for all racial groups. In addition, future studies should continue to characterize socioeconomic factors that may determine choice of treatment modality, as well as genetic factors that might impact survival of patients with HCC.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The IRB waiver for this study was obtained.
References
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010;127:2893-917. [PubMed]
- Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet 2012;379:1245-55. [PubMed]
- Cancer Fact Sheets. Available online: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx (accessed August 9, 2015).
- Altekruse SF, McGlynn KA, Reichman ME. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol 2009;27:1485-91. [PubMed]
- Altekruse SF, Henley SJ, Cucinelli JE, et al. Changing hepatocellular carcinoma incidence and liver cancer mortality rates in the United States. Am J Gastroenterol 2014;109:542-53. [PubMed]
- Kim do Y, Han KH. Epidemiology and surveillance of hepatocellular carcinoma. Liver Cancer 2012;1:2-14. [PubMed]
- Sonnenday CJ, Dimick JB, Schulick RD, et al. Racial and geographic disparities in the utilization of surgical therapy for hepatocellular carcinoma. J Gastrointest Surg 2007;11:1636-46; discussion 1646. [PubMed]
- Mathur AK, Osborne NH, Lynch RJ, et al. Racial/ethnic disparities in access to care and survival for patients with early-stage hepatocellular carcinoma. Arch Surg 2010;145:1158-63. [PubMed]
- Zak Y, Rhoads KF, Visser BC. Predictors of surgical intervention for hepatocellular carcinoma: race, socioeconomic status, and hospital type. Arch Surg 2011;146:778-84. [PubMed]
- Sloane D, Chen H, Howell C. Racial disparity in primary hepatocellular carcinoma: tumor stage at presentation, surgical treatment and survival. J Natl Med Assoc 2006;98:1934-9. [PubMed]
- Luo T, Spolverato G, Johnston F, et al. Factors that determine cancer treatment choice among minority groups. J Oncol Pract 2015;11:259-61. [PubMed]
- Miller BA, Chu KC, Hankey BF, et al. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control 2008;19:227-56.
- SEER Data, 1973-2012. Available online: http://seer.cancer.gov/data/ (accessed July 7, 2015)
- El-Serag HB, Davila JA. Is fibrolamellar carcinoma different from hepatocellular carcinoma? A US population-based study. Hepatology 2004;39:798-803. [PubMed]
- Mayo SC, Mavros MN, Nathan H, et al. Treatment and prognosis of patients with fibrolamellar hepatocellular carcinoma: a national perspective. J Am Coll Surg 2014;218:196-205. [PubMed]
- Wong PY, Xia V, Imagawa DK, et al. Clinical presentation of hepatocellular carcinoma (HCC) in Asian-Americans versus non-Asian-Americans. J Immigr Minor Health 2011;13:842-8. [PubMed]
- Nguyen GC, Thuluvath PJ. Racial disparity in liver disease: Biological, cultural, or socioeconomic factors. Hepatology 2008;47:1058-66. [PubMed]
- Wu CA, Lin SY, So SK, et al. Hepatitis B and liver cancer knowledge and preventive practices among Asian Americans in the San Francisco Bay Area, California. Asian Pac J Cancer Prev 2007;8:127-34. [PubMed]
- Davila JA, Morgan RO, Richardson PA, et al. Use of surveillance for hepatocellular carcinoma among patients with cirrhosis in the United States. Hepatology 2010;52:132-41. [PubMed]
- Page AJ, Cosgrove DC, Philosophe B, et al. Hepatocellular carcinoma: diagnosis, management, and prognosis. Surg Oncol Clin N Am 2014;23:289-311. [PubMed]
- Lin JJ, Mhango G, Wall MM, et al. Cultural factors associated with racial disparities in lung cancer care. Ann Am Thorac Soc 2014;11:489-95. [PubMed]


