Learning curve in laparoscopic liver surgery: a fellow’s perspective
“If I have seen further than others, it is by standing on the shoulders of giants.”—Sir Isaac Newton
Since the 1st report by Reich in 1991, there has been exponential growth in the interest and practice of laparoscopic liver resections (LLR) worldwide. Initially, only wedge resections and minor hepatectomies were attempted (1). However, with increasing experience, better optics and instrumentation, leading surgeons from large academic centers have been performing major hepatectomies, anatomical posterior segment resections, pure donor hepatectomies, and complex combined resections, such as combined major hepatectomy with pancreaticoduodenectomy laparoscopically.
Few reports, however, address the issue of mounting the learning curve in the transition from simple laparoscopic resections to more complex operations. Understandably, the learning curve for laparoscopic liver surgery is difficult to document. The techniques for liver resection differ widely depending on the location and size of the lesion, the need for parenchymal preservation versus anatomical resection, the underlying parenchymal consistency and method of preferred parenchymal transection. Furthermore, there may be the need for concomitant gastrointestinal or major vascular resection.
Each surgeon’s learning curve may be influenced by his or her training background, depending on whether it is from open liver surgery to the laparoscopic approach, or from advanced laparoscopic surgery transitioning to liver surgery. For the open liver surgeon, mastering laparoscopic liver surgery can be a challenge especially with laparoscopic suturing and change in view from the anterior-posterior view of traditional open liver surgery to the caudal-cranial view of laparoscopy. In contrast, the challenge the laparoscopically trained surgeon faces may be understanding liver anatomy and its complex variations which may present a formidable initial learning curve.
Vigano et al. described their learning curve experience, dividing their experience into three groups of 58 patients each, who underwent LLR between 1996 and 2008 (2). In their paper, there were progressive improvements in the conversion rate, operative time, blood loss and morbidity over the time periods. Using conversion rate as their primary outcome (with adjustment for risk factors), they concluded that a learning curve of about 60 patients was required for minor hepatectomies. Abu Hilal et al. on the other hand suggested that improvements in the operative time and median hospital stay could be achieved after only 15 cases for their standardized procedure of laparoscopic left lateral sectionectomy (LLS) (3). In a recent article, Spampinato et al. demonstrated a single surgeon learning curve of only ten cases of major/complex totally LLR with improvements in operative time, median blood loss, transfusion requirement and need for intermittent Pringles maneuver. He attributes this to a solid foundation of advanced training in hepatobiliary and transplant surgery coupled with a fellowship in a high volume tertiary center specializing in laparoscopic and advanced hepatobiliary surgery (4). We recently published our initial experience in LLR and demonstrated that individual surgeon and institution volume were the main risk factors for open conversion after laparoscopic minor hepatectomy during the learning phase, albeit individual surgeon experience was the more significant factor (5). In this experience, based on conversion rates, the learning curve for an individual surgeon was about 15-20 cases for laparoscopic minor liver resection, which was lower than that reported by early studies but similar to more recent studies (2,5,6). This may suggest that with the rapid advancements in surgical technique and equipment for left hemihepatectomy (LH), the learning curve may be shortened when the surgeons collectively share their experience and actively help each other as a team in different phases of each individual’s learning period. Table 1 summarizes several studies on the learning curve for laparoscopic liver surgery.
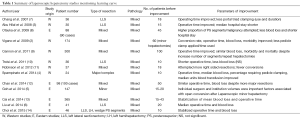
Full table
One of the earliest LLR reported from an Eastern Hepatopancreatobiliary (HPB) unit was by Hashizume and colleagues from Japan in 1995. Here he reported a cirrhotic patient who successfully underwent laparoscopic resection of a 2 cm hepatocellular carcinoma (HCC) in Segment 5 (15). One of the first case series reported from Japan was from Kaneko and colleagues: a series of 11 patients who underwent laparoscopic partial hepatectomy or LLS with only one conversion for bleeding (16). He went on to describe the learning curve for these operations, with an improvement in operative times between the early period [1993-1998] and the later period [1999-2004] (17).
The Louisville consensus statement in 2008 provided international guidelines for laparoscopic liver surgeons and the recently concluded 2nd consensus conference held in Iwate in 2014 further added important evidence with regards to the practice and adoption of this emerging field (18,19). It was recommended in the 1st consensus statement that LLR be limited to solidary lesions (5 cm or less), in anterior segments of the liver (Segments 2,3,4b,5,6) with LLS being standard practice. In the latest consensus from the Iwate meeting, this limitation was cautiously expanded to include all minor resections being standard practice although these are generally taken not to include the “difficult” segments (Segments 1,4a,7,8). There was also a clear trend towards increasing proportion of major resections and complex resections being performed around the world with fewer conversions. Although the level of evidence was still low, it was concluded that in majority of parameters studied, the outcomes were at least not inferior in margin negativity, morbidity, perioperative mortality and overall survival. Furthermore, benefits of minimally invasive surgery (MIS) were seen with superior pain, cosmesis, blood loss and length of stay (19). While most of the evidence for LLR was based on studies without randomized control trials, they consistently show better short-term outcomes without compromise on long-term oncological outcomes. There are two randomized controlled trials underway in Norway (Oslo-CoMet) and Netherlands whose results should give us more insight on these issues (20).
The benefit of being a young laparoscopic liver surgeon in this generation is the availability of literature and videos to learn techniques, compared to our pioneering colleagues. In contrast to the lack of standardized techniques in the early years, there are currently good published techniques on the more common resections such as the LLS and even major hepatectomies (7,21). With increasing experience, technical tips on difficult resections such as isolated posterior segment resections (Segments 7/8), central hepatectomies and caudate resections are being shared (8,22-24). Laparoscopic donor hepatectomy techniques have also been described, although these surgeries are understandably performed only in a handful of high volume transplant centers (25). These are important adjuncts in helping to overcome the learning curve. However, it is important that adoption of these techniques is guided by an experienced surgeon.
Progressing to the more difficult resections should only be attempted after sufficient experience in the simpler resections. Cho et al. compared the outcome after LLR of HCC situated in the antero-lateral segment (Segments 2,3,5,6 and 4b) vs. those in the postero-superior segment (Segments 1,4a,7 and 8), and found that patients with postero-superior segments resected had longer operative time and a tendency towards longer median hospital stay and greater rate of intraoperative transfusion, but with no significant difference in postoperative complications or cancer recurrence (22). A recently published multicenter study in Japan on case selection for pure LLR considered scoring the difficulty of the resection according to low, intermediate and high. This score was calculated based on tumor location, extent of liver resection, tumor size, proximity to major vessel and liver function to provide a score from 1-10 (26). Although yet to be validated by other centers outside of Japan, this paper provided a novel and practical method for predicting the technical difficulty for LLR and may provide a framework to choose resections that they can do laparoscopically consistent with their experience. In the latest consensus statement from Iwate, there was strong recommendations from the jury and expert panel that the validation and application of this novel system be carried out together with a structured training program for further safe adoption of laparoscopic liver surgery.
Personal experience
Coming from a background of predominantly open liver surgery, I decided to embark on an international fellowship in a large tertiary referral center in Australia known for its work in laparoscopic liver surgery. My supervisor Dr. Nicholas O’Rourke, and his unit at the Royal Brisbane Hospital was one of the first to publish their technique of laparoscopic right hepatectomy (27). Since 1999, they have developed an extensive experience in laparoscopic liver surgery, with over 340 laparoscopic resections to date (28,29). There was a good case mix of advanced laparoscopic hepatectomies, laparoscopic pancreatic surgery as well as complex minimally invasive biliary surgery in my training year. During my fellowship, besides laparoscopic hepatobiliary surgery, I was also exposed to advance laparoscopic revisional bariatric surgery as well as upper gastrointestinal surgery. The skills I picked up such as laparoscopic suturing and intra-corporal gastrointestinal anastomoses allowed me to have a broad based training in laparoscopic surgery. This built my confidence in handling LLR, especially in stressful situations when control of bleeding with sutures was required. I also had the opportunity to be involved in the management of many synchronous liver and colorectal resections, since the colorectal unit there was equally accomplished in advanced laparoscopic surgery.
The most important factors in embarking on safe laparoscopic liver surgery, in my experience, were the appreciation of liver anatomy from the caudal cranial view, learning laparoscopic haemostatic control and developing familiarity in using the laparoscopic ultrasound. In the initial learning process, many hours were spent assisting in laparoscopic surgeries and watching available videos to understand the various different approaches to major and minor resections in the caudal cranial perspective. While this caudal cranial view afforded excellent visualization of the infra-hepatic tunnel for securing the short hepatic veins, the orientation of the resection plane can be confusing, and access to the major hepatic veins difficult. It is crucial to be able to control bleeding and the ability to laparoscopically suture quickly at awkward locations is a skill that should be practiced till proficient even before embarking on the 1st LLR without senior supervision. The use of the laparoscopic ultrasound was a difficult technique to learn but was indispensable to continuously check on resection line, vascular anatomy deep in the liver and also margin control especially for non-anatomical resections. While there are many known techniques of parenchymal transection with a variety of energy devices, it was important to learn and be familiar with one technique consistently before embarking on other methods. Although pure laparoscopy was generally preferred, before starting operations, a potential site for hybrid or hand port was routinely marked for conversion should there be situations of difficult bleeding control or failure to progress. I did not view conversion as a failure but a necessity especially when there are concerns about oncological clearance.
After returning to Singapore, I quickly began to develop a laparoscopic liver surgery program in my institution. Starting out, it was prudent to perform only simple wedge resections of anterolateral segments and LLS within the guidelines provided by the Louisville consensus statement for minor resections. This allowed me to train my team of junior surgeons and nursing staff under less technically demanding conditions, whilst avoiding the risk of significant patient morbidity during the early days of the program.
There was also cross collaboration with other colleagues from different institutions in Singapore, one of whom was a HPB surgeon (SYL) who did a laparoscopic and liver transplant fellowship in North America with Prof. Daniel Cherqui and subsequently a surgical oncology fellowship at Memorial Sloan Kettering Cancer Center (MSKCC). The first fellowship allowed him to not only learn first-hand from one of the pioneers of laparoscopic liver surgery but provided him an unique learning opportunity and interaction with a young attending at the same unit, who was Prof. Cherqui’s fellow in Paris a few years prior. This provided valuable lessons and insights how one should cautiously and appropriately embark on a laparoscopic HPB practice. The availability of an experienced mentor in challenging cases was technically helpful and morally encouraging in and out of the operating room. It also provided a unique environment where he saw how laparoscopic surgery can be safely integrated into living donor hepatectomies to decrease donor morbidity (25). The latter MSKCC fellowship was synergistic as it allowed him to experience another perspective—the role of MIS in HPB surgical oncology. Being a cancer center, in his opinion, MSKCC did not jump on the bandwagon of pursing MIS surgery right from the start and its adoption of MIS was more calculated than other high volume tertiary centers because of the rightful concerns of MIS compromising the principles of surgical oncology (30,31). As Dr. Blake Cady once elegantly said: “In the land of Surgical Oncology, biology is King; selection of case is Queen, and the technical details of surgical procedures are princes and princesses of the realm who frequently try to overthrow the powerful forces of the King and Queen, usually to no long-term avail, although with some temporary apparent victories.” Nonetheless, because of potential benefits, culminating experience and convincing data, MIS and surgical oncology proves no longer to be mutually exclusive as long as patients are well selected and surgery performed by experienced teams (32).
In our initial experience, we worked together for major and complex hepatectomies operating with at least one other experienced laparoscopic liver surgeon (CYC). This was crucial in bringing different techniques learnt from our various training backgrounds and working to adapt these techniques to our local patients. In the Western institutions that we worked in, the majority of the resections were for colorectal liver metastases where the challenge was operating on post chemotherapy liver with the principle of parenchymal preservation. In addition, there were important lessons learnt in terms of multidisciplinary discussion and surgical approaches to combined colorectal and liver resections. In our local Asian population, we see a larger proportion of cases with HCC in cirrhotic livers (5). Besides chronic liver disease, they present additional challenges of portal hypertension with concurrent clinical coagulopathy and increased risk of bleeding. Furthermore they tolerate complications less readily and have a need for a larger future liver remnant. This has required us to adapt some techniques of liver mobilization and parenchymal transection in the setting of cirrhosis and portal hypertension. While our technique for parenchymal transection has been with hot “kelly-clysis” with a bipolar vessel sealing device, we have found the Calvitron Ultrasonic Surgical Aspirator (CUSA) (Tyco Healthcare, Mansfield, MA) as an important adjunct for careful dissection of lesions near major vascular pedicles. A roticulating energy device was also useful for non-anatomical resections and lesions higher up in the dome of the liver together with a flexible tip endoscope.
In conclusion, a solid background in open liver surgery coupled with robust training in a high volume subspecialty laparoscopic centre provided a good foundation for starting laparoscopic liver surgery. Adaptation of techniques to the local context is crucial and inter-institutional collaboration allows synergistic development of skills to mount the learning curve for more complex laparoscopic hepatobiliary surgery. The challenge remains in selecting the appropriate patient for LLR and having better guidelines and scoring systems to anticipate the difficulty of resection would undoubtedly enable us to achieve this aim.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Reich H, McGlynn F, DeCaprio J, et al. Laparoscopic excision of benign liver lesions. Obstet Gynecol 1991;78:956-8. [PubMed]
- Vigano L, Laurent A, Tayar C, et al. The learning curve in laparoscopic liver resection: improved feasibility and reproducibility. Ann Surg 2009;250:772-82. [PubMed]
- Abu Hilal M, Pearce NW. Laparoscopic left lateral liver sectionectomy: a safe, efficient, reproducible technique. Dig Surg 2008;25:305-8. [PubMed]
- Spampinato MG, Arvanitakis M, Puleo F, et al. Assessing the Learning Curve for Totally Laparoscopic Major-Complex Liver Resections: A Single Hepatobiliary Surgeon Experience. Surg Laparosc Endosc Percutan Tech 2015;25:e45-50. [PubMed]
- Goh BK, Chan CY, Wong JS, et al. Factors associated with and outcomes of open conversion after laparoscopic minor hepatectomy: initial experience at a single institution. Surg Endosc 2015;29:2636-42. [PubMed]
- Cai X, Li Z, Zhang Y, et al. Laparoscopic liver resection and the learning curve: a 14-year, single-center experience. Surg Endosc 2014;28:1334-41. [PubMed]
- Otsuka Y, Tsuchiya M, Maeda T, et al. Laparoscopic hepatectomy for liver tumors: proposals for standardization. J Hepatobiliary Pancreat Surg 2009;16:720-5. [PubMed]
- Ishizawa T, Gumbs AA, Kokudo N, et al. Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg 2012;256:959-64. [PubMed]
- Cannon RM, Brock GN, Marvin MR, et al. Laparoscopic liver resection: an examination of our first 300 patients. J Am Coll Surg 2011;213:501-7. [PubMed]
- Troisi RI, Van Huysse J, Berrevoet F, et al. Evolution of laparoscopic left lateral sectionectomy without the Pringle maneuver: through resection of benign and malignant tumors to living liver donation. Surg Endosc 2011;25:79-87. [PubMed]
- Robinson SM, Hui KY, Amer A, et al. Laparoscopic liver resection: is there a learning curve? Dig Surg 2012;29:62-9. [PubMed]
- Chan FK, Cheng KC, Yeung YP. Laparoscopic liver resection: lessons learnt after 100 cases. Hong Kong Med J 2014;20:386-92. [PubMed]
- Liu W, Wang Q, Huang J, et al. Laparoscopic left lateral sectionectomy -the learning curve and the role of left hepatic inflow occlusion. Hepatogastroenterology 2014;61:417-21. [PubMed]
- Choi SH, Choi GH, Han DH, et al. Laparoscopic liver resection using a rubber band retraction technique: usefulness and perioperative outcome in 100 consecutive cases. Surg Endosc 2015;29:387-97. [PubMed]
- Hashizume M, Takenaka K, Yanaga K, et al. Laparoscopic hepatic resection for hepatocellular carcinoma. Surg Endosc 1995;9:1289-91. [PubMed]
- Kaneko H, Takagi S, Shiba T. Laparoscopic partial hepatectomy and left lateral segmentectomy: technique and results of a clinical series. Surgery 1996;120:468-75. [PubMed]
- Kaneko H. Laparoscopic hepatectomy: indications and outcomes. J Hepatobiliary Pancreat Surg 2005;12:438-43. [PubMed]
- Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825-30. [PubMed]
- Wakabayashi G, Chiriquí D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in morioka. Ann Surg 2015;261:619-29. [PubMed]
- van Dam RM, Wong-Lun-Hing EM, van Breukelen GJ, et al. Open versus laparoscopic left lateral hepatic sectionectomy within an enhanced recovery ERAS® programme (ORANGE II-trial): study protocol for a randomised controlled trial. Trials 2012;13:54. [PubMed]
- Chang S, Laurent A, Tayar C, et al. Laparoscopy as a routine approach for left lateral sectionectomy. Br J Surg 2007;94:58-63. [PubMed]
- Cho JY, Han HS, Yoon YS, et al. Feasibility of laparoscopic liver resection for tumors located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumor location. Surgery 2008;144:32-8. [PubMed]
- Conrad C, Ogiso S, Inoue Y, et al. Laparoscopic parenchymal-sparing liver resection of lesions in the central segments: feasible, safe, and effective. Surg Endosc 2015;29:2410-7. [PubMed]
- Gringeri E, Boetto R, Bassi D, et al. Totally laparoscopic caudate lobe resection: technical aspects and literature review. Surg Laparosc Endosc Percutan Tech 2014;24:e233-6. [PubMed]
- Samstein B, Cherqui D, Rotellar F, et al. Totally laparoscopic full left hepatectomy for living donor liver transplantation in adolescents and adults. Am J Transplant 2013;13:2462-6. [PubMed]
- Ban D, Tanabe M, Ito H, et al. A novel difficulty scoring system for laparoscopic liver resection. J Hepatobiliary Pancreat Sci 2014;21:745-53. [PubMed]
- O'Rourke N, Fielding G. Laparoscopic right hepatectomy: surgical technique. J Gastrointest Surg 2004;8:213-6. [PubMed]
- Chiow AK, Lewin J, Manoharan B, et al. Intercostal and transthoracic trocars enable easier laparoscopic resection of dome liver lesions. HPB (Oxford) 2015;17:299-303. [PubMed]
- O'Rourke N, Shaw I, Nathanson L, et al. Laparoscopic resection of hepatic colorectal metastases. HPB (Oxford) 2004;6:230-5. [PubMed]
- Ito K, Ito H, Are C, et al. Laparoscopic versus open liver resection: a matched-pair case control study. J Gastrointest Surg 2009;13:2276-83. [PubMed]
- Fong Y, Jarnagin W, Conlon KC, et al. Hand-assisted laparoscopic liver resection: lessons from an initial experience. Arch Surg 2000;135:854-9. [PubMed]
- Lee SY, Allen PJ, Sadot E, et al. Distal pancreatectomy: a single institution's experience in open, laparoscopic and robotic approaches. J Am Coll Surg 2015;220:18-27. [PubMed]


