Pancreatic fistula and postoperative pancreatitis after pancreatoduodenectomy for pancreatic cancer
Introduction
Pancreatoduodenectomy (PD) has its indication of radical intent in the treatment of periampulary malignant tumors as cephalopancreatic neoplasia, distal cholangiocarcinoma or ampuloma. PD managing to provide a 5-year survival of 31.4% for tumors diagnosed in stage I and only 2.8% for stage IV with a median of 24.1 and 4.5 months respectively (1). In patients with unresectable adenocarcinoma 5-year survival reach only 0.6% for stage IV with a median survival of 2.5 months and 3.8% for stage I with a median of 6.8 months. Radical resection is the only chance for patients with this tumor. Unfortunately only 15-20% of them are suitable for it.
Mortality of this type of resection has intermediate risk to compare to total pancreatectomy with highest and to distal pancreatectomy with lowest risk. Retrospective review from a prominent high volume cancer center revealed 30-day mortality rates of 4.9% in the 1980s, 1.5% in the 1990s and 1.3% in the 2000s (2). By the Nationwide Inpatient Sample for 1994-1999 Birkmeyer et al. demonstrated wide variation in perioperative mortality based on hospital volume: 17.6% for low volume compared to 3.8% for high volume (3).
Complications after PD affect a large part of patients and include a variety of clinical entities—internal (as pneumonia, cardiovascular events, infection and others) as well as surgical [bleeding, pancreatic fistula (PF), postoperative pancreatitis (PP), infection-sepsis and others]. The high rate of complications is due to multiple factors as comorbidity, technical complexity of the operation, frail patient population and remains as high as 31-60% (4).
The aim of this review is to present the occurrence of PF and PP, the possibilities of their differentiation and some aspects of treatment after PD as well as to present some aspects of the possibilities to differentiate PH and PP in our retrospective study.
Pancreatic fistula (PF)
PF is the most feared complication after PD, being considered the “Achilles’ heel” of this procedure (5). In spite of previous studies with outstanding results with almost no need for reoperation (6), actual rate of PF grade “C”—severe—(7) requiring operative re-intervention varies between 5% and 20% with mortality rate nearly 40% (8).
Definition
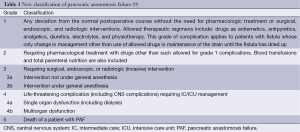
There is no universally accepted definition of PF. Most of them rely on amylase content of the effluent from intraabdominal drain. International study group of PF (ISGPF) organized by Bassi et al. (7) extended definition to standardizing of postoperative treatment by the adoption and by the modification the definition based on clinical impact on the patient hospital course and the outcome and graded PF into A, B, C. The grading was based on nine clinical criteria: patient’s condition, use of specific treatment, US and/or CT findings, persistent drainage >3 weeks, reoperation, signs of infection, sepsis, readmissions and death. Strasberg et al. proposed intraabdominal collection with hemorrhage and peritonitis are also the result of PF (9) (Table 1).
Risk factors for PF
Multivariate logistic regression analysis showed that none of the general risk factors as age, gender, history of jaundice, preoperative nutrition, type of resection and the length of postoperative stay seemed to be associated with PH (10,11). Two intraoperative risk factors—pancreatic duct size and parenchyma texture of the remnant pancreas—were found to be significantly associated with PF. Pancreatic duct size >3 mm means only 4.88% of PF, and 38.1% in pancreatic duct size <3 mm respectively. PH rate was less than 3% in hard pancreatic tissue meanwhile in soft tissue reached more than 32%. French multicentric retrospective survey on PD for ductal adenocarcinoma found that a soft pancreatic parenchyma, the absence of preoperative diabetes, pancreaticojejunostomy and low volume centers were independent risk factors for PF (12). Although anastomotic technique was not a significant factor, PH rate was much less in cases of duct-to-mucosa pancreaticojejunostomy (10,13,14). On the other hand PH risk score for prediction of clinically-relevant PH after PD reflected intraoperative blood loss (13). There are other factors apart from technical consideration, of which increased intraoperative blood loss—more advanced stages of disease requiring portal or superior mesenteric vein resection, patient obesity, jaundice associated coagulopathy and others (11).
Moreover careful consideration should be given to the larger pancreatic stumps, wide pancreatic remnant mobilization, and the duct decentralization on the stump in anteroposterior axis (15).
Preventive measures
Occlusion of pancreatic duct
To prevent complications following PD especially the development of PF various techniques of managing the pancreatic remnant have been proposed (11). Occlusion of the pancreatic duct (chemical occlusion or simple duct ligation) compared with pancreaticojejunostomy there is no significant difference found in the postoperative complications, mortality and exocrine insufficiency. Moreover there were significantly more patients with diabetes mellitus in the duct occlusion group. So there is no evidence to show that pancreaticojejunostomy can be replaced by pancreatic duct occlusion (16).
Pancreaticogastrostomy
Four RCTs comparing pancreaticogastrostomy to pancreaticojejunostomy have failed to show any significant difference regarding to PF ratio, postoperative complications or mortality (17-20). The type of anastomotic fashion plays no role for the risk of PF. Results of one RCT has showed significantly lower rate and severity of PF after pancreaticogastrostomy compared to pancreaticojejunostomy (21). A prospective RCT by Bassi et al. revealed no significant difference in PF ratio between duct–to-mucosa anastomosis and single layer end-to-side pancreaticojejunostomy (22). The use of isolated Roux-en-Y pancreaticojejunostomy cannot prevent the development of PF formation (20,23).
Total pancreatectomy
Total pancreatectomy allows not only more extensive lympfadenectomy and decreases the risk of positive resection margins but also obviates a leak from pancreatic anastomosis. This type of procedures is however associated with the development of diabetes mellitus, decreasing of immunity and loss of pancreatic exocrine function. So indication for total pancreatectomy is not corresponding to routine treatment of localized ductal adenocarcinoma of the head of pancreas (24).
Based on the current evidence it is unclear whether drainage of pancreatic duct with a stent (internal or external) can reduce PF rate (25,26).
Pharmacologic prevention
There were optimistic results of the multicentric study regarding to the role of Octreotide in the prevention of postoperative complications following pancreatic resection from the 90’s showing reducing of the occurrence of the typical postoperative complications (27). Current single-center, randomized, double-blind trial of perioperative subcutaneous pasireotide in patients undergoing either PD or distal pancreatectomy showed similar results. Authors presented that the perioperative treatment with pasireotide decreased the rate of clinically significant postoperative PF, leak, or abscess (28).
According to the actual literature the administration of Octreotide by principle is not recommended but only in the case of low consistency pancreatic parenchyma or when intraoperative handling of the pancreatic stump is more aggressive (10). Somatostatin administration may have reduced the pancreas edema, protected the normal tissues and improved the anastomosis quality, but on a daily basis, the abdominal drainage fluid is not affected without any difference between preoperative and postoperative use (29). Moreover there is no statistical difference in the incidence of PF between the patients who received the prophylactic use of octreotide after surgery and the patients who did not somatostatin therapy (30).
Drain removal and other preventions
There is no standard regarding to the best time when the intraabdominal drain should be removed. The most surgeons indicate drainage removal once the output of amylase-rich fluid is low (31). Until now, there has been no consensus on the optimal timing of the removal of prophylactic drainage after pancreatic surgery in general. The similar situation is associated with poor or no agreement to the type of nutrition, use of antibiotics, imaging strategy and hospital discharge (32).
Treatment approaches
The current treatment depends on the grade of PF. It is noteworthy that 70% of PH resolves spontaneously (33). The best strategy for the management of PF is still highly debated. Actual rate of PF grade C requiring a relaparotomy varies between 5-20% even in experienced center with mortality rate as high as 39% (4,8). Different strategies include both preservation of the pancreatic remnant and a completion pancreatectomy (34). Pancreatectomy avoids further PF but leads to complete pancreatic insufficiency and to “brittle” diabetes (35). Preserving approach—debridement and drainage of the pancreatic region or resection the dehiscent jejunal loop followed by the occlusion of the main pancreatic duct—is technically easier and has the advantage of maintaining pancreatic function but on the other hand leads to the risk of a persistent PH. Balzano et al. presented better results with completion pancreatectomy with splenectomy in the case of PH grade C with autologous islet transplantation reducing the metabolic consequences of total pancreatectomy (36). Moreover there is experience with other methods—the conversion to pancreaticogastrostomy and the bridging stent technique but without evidence whether drainage of the pancreatic duct with a stent can reduce PF rate after PD (37). Finally there is also the experience with resection of dehiscent jejunal loop and drainage of pancreatic region followed by gastrofistulostomy (38).
Acute postoperative pancreatitis (PP)
PP is a less frequent but very serious surgical complication with often fatal results. It is most often seen following surgery on the pancreas itself, but in rare cases has also been described after surgical procedures on organs very distant from the pancreas. The occurrence of PP according to Carter from 1956 depends upon the following condition (39): mechanical injury direct to the pancreas and especially to the pancreatic ducts, vascular conditions, spasm of the sphincter of Oddi and stagnation of duodenal contents.
The incidence of PP reported in the literature is approximately 8-10%, following PD ranges from 1.9-50% (40). But to analyze PP ratio by literature is difficult: PP is mostly not evaluated as a separate complication of PD but in the range of PH (40). Contrary to acute pancreatitis with 5-15% mortality, the mortality of PP is more than 30% (41).
Diagnosis
PP is clinically defined as abdominal pain which develops during the postoperative course with a concurrent two- to three-fold increase in the levels of specific pancreatic enzymes in the blood. A non-standard postoperative course accompanied by pain, distension of the abdominal muscles, prolonged paralytic ileus and cloudy, often brownish, discharge from the drains may signify developing PP (26,42,43). Evaluation may however be complicated by the development of benign postoperative hyperamylasemia and the subjective perception of postoperative pain. Clinical symptoms may be hidden, especially if the patient remains under analgosedation, or even on artificial lung ventilation, after a long operation with greater blood loss. The first warning sign of the development of PP may be progressive circulatory instability, especially in patients with replenished blood supply (26). Early diagnosis of PP based on clinical and laboratory results is very difficult from standard currently performed examinations, as is the evaluation of preoperative findings during reoperation, especially after a longer interval from the primary operation.
Nonetheless a similar condition may also be caused by other postoperative complications. In a study by Wilson et al. (44) which clinically evaluated the postoperative course PP was only diagnosed at autopsy in 10 of 11 cases. Operative findings on revision also do not always correlate with the results of laboratory and imaging examinations.
Pancreatic leak from PJA or PGA and peripancreatic abscess may be clinical signs of PP. They may however also develop due to technical error during sewing of the anastomosis, where edge necrosis may occur in an otherwise undisturbed glandular parenchyma. During surgical revision in a postoperatively changed terrain, pathological changes in the remaining pancreas and its surroundings are often difficult to evaluate due to signs of superficial tissue digestion and the presence of necrosis, which develop due to digestion by activated pancreatic juice. Postoperative changes in cases of PF may easily be misinterpreted for signs of PP and vice-versa.
Regarding laboratory analysis, in addition to values of amylase, lipase and trypsin levels, Büchler et al. also favors analysis of CRP and calcium levels (45). In recent years, diagnosis of PP has most often been reliant on CRP level along with the result of spiral contrast CT examination, where necrotic changes in the parenchyma are evaluated according to the Balthazar classification (46). In accordance with current literary findings, CRP levels best reflect the development and course of the disease. In contrast, CT examination performed prior to surgical revision has not shown to be beneficial in terms of evaluating changes in the pancreatic gland.
Treatment approaches
PJA disconnection and drainage procedures during surgical revision after PD in cases of PP are usually insufficient and do not lead to a better prognosis. An appropriate, although risky, solution during early revision with suspicion of PP is a completion pancreatectomy with splenectomy. However, after late revisions in an operating field devastated by pancreatitis, the mortality of patients after completion pancreatectomy nears 100%, according to most authors (47,48). Is it desirable to proceed with the completion pancreatectomy soon after the primary procedure (34)? However to perform a completion pancreatectomy in a patient with PF type C may be an unwarranted procedure, unjustifiably risky with subsequent significant worsening of quality of life. Early diagnosis of PP may therefore be a key moment in the treatment of PH type C in patients after PD.
Base on the current literature, very few firm statements can be made: the criteria for drain removal, imaging strategy and timing of hospital discharge in patients with PF remain unclear (31). In the case of PP after PD treatment strategy is unclear yet and available standard is lacking.
Our own experience
We retrospectively evaluated the postoperative clinical course, and radiological and laboratory data of 7/160 patients underwent PD in the period of 2007-2011 in our institution for ductal adenocarcinoma of the head of pancreas and died during primary hospitalization because of PF type C with autopsy findings of PP in four cases (49). We compared this group of 4 (2.5%) patients to the group of 10 (6.25%) patients with only a pancreatic leak type C and 12 (7.5%) patients with an uncomplicated clinical course. None of the patients with PP survived. We found significantly higher levels of serum pancreatic amylase on the 1st postoperative day (POD) in 3 of these patients compared to the other groups. Significantly increasing levels of CRP during the first five POD were observed in 75% of these patients. Retrospectively analyzed contrast CT scans up to the 5th POD did not show PP. Only 1 patient had findings of PP type E according to Balthazar on CT scan performed on the 9th POD.
Results commentary
A basic aim of our study was to confirm or rule out a diagnosis of PP in the interval from the primary surgical procedure to the surgical revision, with respect to our standard type of surgical procedure (disconnection and closure of the feature stump and peripancreatic drainage). Our retrospective evaluation showed that we were mistaken in almost half of the patients. Subsequent decision to perform a disconnection of the pancreatojejunostomy with drainage of the resected area with planned external PF did not reflect the current view on treatment of this complication. This error, in both diagnosis and type of surgical revision, has also been presented by other authors, who came to very similar conclusions based on retrospective analyses (50,51). Completion pancreatectomy can be of significant benefit when performed as soon as possible after diagnosis of potentially fatal PP (52). The longer the interval between primary operation and surgical revision, the lower the chance of performing completion pancreatectomy without endangering the life of the patient. Due to the gradual postoperative development of inflammatory peripancreatic infiltrate, the procedure becomes intolerable for the patient. In any case, the decision to perform completion pancreatectomy is very difficult for the surgeon.
In our set of patients who died in direct association with a serious postoperative pancreatic leak from the pancreaticojejunostomy, PP occurred in 4 out of 7 cases (57%) based on autopsy histological findings. All of these patients were suspected of having PP based on macroscopic findings during revision surgery.
If we retrospectively evaluate our patient group and our reaction to the obtained values—markers—of PP, it is necessary to state that we rather underestimated the increasing values and was of the opinion that the values reflect developing pancreatic leak and that we have time and will observe the patient. We evidently missed the opportunity to perform early surgical revision and remove the remaining pancreas.
Another discovery was the evaluation of the postoperative finding on the remaining pancreas. We attributed superficial necroses to developing PP; autopsy findings, however, did not confirm PP. Evidently these were superficial changes caused by digestion of pancreatic tissue by activated pancreatic juice from PJA dehiscence. In accordance with other authors, we do not consider feature soft biopsy to be of value.
Prior CT examinations did not describe structural changes in the pancreas in any of the four cases of autopsy-confirmed PP, not even on retrospective evaluation.
The results of our retrospective study confirmed the following:
- An abrupt increase in values of serum amylase and CRP from the 1st POD to 5th POD is indicative of the development of PP following PD for ductal adenocarcinoma;
- CT examination may not be beneficial in diagnosing this complication;
- When life-threatening PP is diagnosed, a completion pancreatectomy is recommended. The decision depends on the surgeon’s experience;
- In some patients, PP may not be confirmed on biopsy or autopsy; changes on the remaining pancreas may only be superficial, caused by digestion of activated pancreatic juice leaking from dehiscence of the pancreaticojejunostomy.
Cost of pancreatic fistula (PF)
Patients who experience any complications after pancreatic surgery are associated with a three-fold increase in costs over those without complications (53). It is of note that one of the most serious postoperative surgical complications is PF type C either as a consequence or independently from PP. The hospital stay of these patients is significantly longer than that of patients without PF (53). A median total cost of the treatment depends on the type of PF: A, B and C—100%, 170%, 620% respectively. There is no significant difference in total cost between patients without PF and with PF type A (54).
Conclusions
The most serious complication after PD is PF type C, either as a consequence or independently from PP. Differentiating between these two types of complications is difficult. Meantime PF type C is indication to operative revision with mostly drainage procedure which is obviously not much technically demanding, there are no definite guidelines on how to proceed in PP. Therefore the surgeon’s experience determines not only whether PP will be diagnosed early enough and will be differentiated from PF without PP, but also whether a completion pancreatectomy will be performed in indicated cases.
Patients who experience any complications after pancreatic surgery are associated with a three-fold increase in costs over those without complications.
Acknowledgements
Supported by grant IGA MZCR NT 13 263 and by project of MO1012.
Disclosure: The authors declare no conflict of interest.
References
- Bilimoria KY, Bentrem DJ, Ko CY, et al. Validation of the 6th edition AJCC Pancreatic Cancer Staging System: report from the National Cancer Database. Cancer 2007;110:738-44.
- Winter JM, Brennan MF, Tang LH, et al. Survival after resection of pancreatic adenocarcinoma: results from a single institution over three decades. Ann Surg Oncol 2012;19:169-75. [PubMed]
- Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med 2002;346:1128-37. [PubMed]
- Standop J, Glowka T, Schmitz V, et al. Operative re-intervention following pancreatic head resection: indications and outcome. J Gastrointest Surg 2009;13:1503-9. [PubMed]
- Stojadinovic A, Brooks A, Hoos A, et al. An evidence-based approach to the surgical management of resectable pancreatic adenocarcinoma. J Am Coll Surg 2003;196:954-64. [PubMed]
- Büchler MW, Wagner M, Schmied BM, et al. Changes in morbidity after pancreatic resection: toward the end of completion pancreatectomy. Arch Surg 2003;138:1310-4; discussion 1315. [PubMed]
- Bassi C, Dervenis C, Butturini G, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005;138:8-13. [PubMed]
- Fuks D, Piessen G, Huet E, et al. Life-threatening postoperative pancreatic fistula (grade C) after pancreaticoduodenectomy: incidence, prognosis, and risk factors. Am J Surg 2009;197:702-9. [PubMed]
- Strasberg SM, Linehan DC, Clavien PA, et al. Proposal for definition and severity grading of pancreatic anastomosis failure and pancreatic occlusion failure. Surgery 2007;141:420-6. [PubMed]
- Werner J, Büchler MW. Resectional techniques: Pancreaticoduodenectomy, distal pancreatectomy, segmental pancreatectomy, total pancreatectomy, and transduodenal resection of the papilla of Vater. In: Jarnagin WR, Blumgart LH. eds. Blumgart’s Surgery of the Liver, Pancreas and Biliary Tract. 5th ed. Philadelphia: Saunders, 2013.
- Machado NO. Pancreatic fistula after pancreatectomy: definitions, risk factors, preventive measures, and management-review. Int J Surg Oncol 2012;2012:602478.
- Addeo P, Delpero JR, Paye F, et al. Pancreatic fistula after a pancreaticoduodenectomy for ductal adenocarcinoma and its association with morbidity: a multicentre study of the French Surgical Association. HPB (Oxford) 2014;16:46-55. [PubMed]
- Yang YM, Tian XD, Zhuang Y, et al. Risk factors of pancreatic leakage after pancreaticoduodenectomy. World J Gastroenterol 2005;11:2456-61. [PubMed]
- De Carlis L, Ferla F, Di Sandro S, et al. Pancreatico-duodenectomy and postoperative pancreatic fistula: risk factors and technical considerations in a specialized HPB center. Updates Surg 2014;66:145-50. [PubMed]
- Ridolfi C, Angiolini MR, Gavazzi F, et al. Morphohistological features of pancreatic stump are the main determinant of pancreatic fistula after pancreatoduodenectomy. Biomed Res Int 2014;2014:641239.
- Tran K, Van Eijck C, Di Carlo V, et al. Occlusion of the pancreatic duct versus pancreaticojejunostomy: a prospective randomized trial. Ann Surg 2002;236:422-8; discussion 428. [PubMed]
- Yeo CJ, Cameron JL, Maher MM, et al. A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg 1995;222:580-8; discussion 588-92. [PubMed]
- Duffas JP, Suc B, Msika S, et al. A controlled randomized multicenter trial of pancreatogastrostomy or pancreatojejunostomy after pancreatoduodenectomy. Am J Surg 2005;189:720-9. [PubMed]
- Bassi C, Falconi M, Molinari E, et al. Reconstruction by pancreaticojejunostomy versus pancreaticogastrostomy following pancreatectomy: results of a comparative study. Ann Surg 2005;242:767-71, discussion 771-3. [PubMed]
- El Nakeeb A, Hamdy E, Sultan AM, et al. Isolated Roux loop pancreaticojejunostomy versus pancreaticogastrostomy after pancreaticoduodenectomy: a prospective randomized study. HPB (Oxford) 2014;16:713-22. [PubMed]
- Figueras J, Sabater L, Planellas P, et al. Randomized clinical trial of pancreaticogastrostomy versus pancreaticojejunostomy on the rate and severity of pancreatic fistula after pancreaticoduodenectomy. Br J Surg 2013;100:1597-605. [PubMed]
- Bassi C, Falconi M, Molinari E, et al. Duct-to-mucosa versus end-to-side pancreaticojejunostomy reconstruction after pancreaticoduodenectomy: results of a prospective randomized trial. Surgery 2003;134:766-71. [PubMed]
- Lai EC, Lau SH, Lau WY, et al. Measures to prevent pancreatic fistula after pancreatoduodenectomy: a comprehensive review. Arch Surg 2009;144:1074-80. [PubMed]
- Karpoff HM, Klimstra DS, Brennan MF, et al. Results of total pancreatectomy for adenocarcinoma of the pancreas. Arch Surg 2001;136:44-7; discussion 48. [PubMed]
- Winter JM, Cameron JL, Campbell KA, et al. Does pancreatic duct stenting decrease the rate of pancreatic fistula following pancreaticoduodenectomy? Results of a prospective randomized trial. J Gastrointest Surg 2006;10:1280-90; discussion 1290. [PubMed]
- Ohwada S, Tanahashi Y, Ogawa T, et al. In situ vs ex situ pancreatic duct stents of duct-to-mucosa pancreaticojejunostomy after pancreaticoduodenectomy with billroth I-type reconstruction. Arch Surg 2002;137:1289-93. [PubMed]
- Büchler M, Friess H, Klempa I, et al. Role of octreotide in the prevention of postoperative complications following pancreatic resection. Am J Surg 1992;163:125-30; discussion 130-1. [PubMed]
- Allen PJ, Gönen M, Brennan MF, et al. Pasireotide for postoperative pancreatic fistula. N Engl J Med 2014;370:2014-22. [PubMed]
- Wang W, Tian B, Babu SR, et al. Randomized, placebo-controlled study of the efficacy of preoperative somatostatin administration in the prevention of postoperative complications following pancreaticoduodenectomy. Hepatogastroenterology 2013;60:400-5. [PubMed]
- Connor S, Alexakis N, Garden OJ, et al. Meta-analysis of the value of somatostatin and its analogues in reducing complications associated with pancreatic surgery. Br J Surg 2005;92:1059-67. [PubMed]
- Giovinazzo F, Butturini G, Salvia R, et al. Drain management after pancreatic resection: state of the art. J Hepatobiliary Pancreat Sci 2011. [Epub ahead of print].
- Melloul E, Raptis DA, Clavien PA, et al. Poor level of agreement on the management of postoperative pancreatic fistula: results of an international survey. HPB (Oxford) 2013;15:307-14. [PubMed]
- González-Pinto I, González EM. Optimising the treatment of upper gastrointestinal fistulae. Gut 2001;49 Suppl 4:iv22-31. [PubMed]
- Dellaportas D, Tympa A, Nastos C, et al. An ongoing dispute in the management of severe pancreatic fistula: Pancreatospleenectomy or not? World J Gastrointest Surg 2010;2:381-4. [PubMed]
- Maeda H, Hanazaki K. Pancreatogenic diabetes after pancreatic resection. Pancreatology 2011;11:268-76. [PubMed]
- Balzano G, Pecorelli N, Piemonti L, et al. Relaparotomy for a pancreatic fistula after a pancreaticoduodenectomy: a comparison of different surgical strategies. HPB (Oxford) 2014;16:40-5. [PubMed]
- Kent TS, Callery MP, Vollmer CM Jr. The bridge stent technique for salvage of pancreaticojejunal anastomotic dehiscence. HPB (Oxford) 2010;12:577-82. [PubMed]
- Rudiš J, Ryska M. Postoperative pancreatic fistula management by gastrofistuloanastomosis - a set of case reports. Rozhl Chir 2012;91:620-4. [PubMed]
- Carter Ae. Post-operative pancreatitis. Postgrad Med J 1956;32:248-58. [PubMed]
- Kriger AG, Kubishkin VA, Karmazanovskiĭ GG, et al. The postoperative pancreatitis after the pancreatic surgery. Khirurgiia (Mosk) 2012;14-9. [PubMed]
- Imrie CW, Dickson AP. Postoperative pancreatitis. In: Howard JM, Jordan GL, Reber HA. eds. Surgical diseases of the pancreas. Philadelphia: Lea and Febiger, 1987:332-41.
- Z’gragen K, Uhl W, Büchler MW. Acute postoperative pancreatitis. In: Beger HG, Warshaw AL, Büchler MW, et al. eds. The Pancreas. Oxford: Blackwell Science, 1998:283-90.
- Z’graggen K, Aronsky D, Maurer CA, et al. Acute postoperative pancreatitis after laparoscopic cholecystectomy. Results of the Prospective Swiss Association of Laparoscopic and Thoracoscopic Surgery Study. Arch Surg 1997;132:1026-30; discussion 1031. [PubMed]
- Wilson C, Imrie CW. Deaths from acute pancreatitis: why do we miss the diagnosis so frequently? Int J Pancreatol 1988;3:273-81. [PubMed]
- Büchler MW, Gloor B, Müller CA, et al. Acute necrotizing pancreatitis: treatment strategy according to the status of infection. Ann Surg 2000;232:619-26. [PubMed]
- Balthazar EJ. CT diagnosis and staging of acute pancreatitis. Radiol Clin North Am 1989;27:19-37. [PubMed]
- van Berge Henegouwen MI, De Wit LT, Van Gulik TM, et al. Incidence, risk factors, and treatment of pancreatic leakage after pancreaticoduodenectomy: drainage versus resection of the pancreatic remnant. J Am Coll Surg 1997;185:18-24. [PubMed]
- Smith CD, Sarr MG, vanHeerden JA. Completion pancreatectomy following pancreaticoduodenectomy: clinical experience. World J Surg 1992;16:521-4. [PubMed]
- Rudis J, Ryska M. Pancreatic leakage and acute postoperative pancreatitis after proximal pancreatoduodenectomy. Rozhl Chir 2014;93:380-5.
- Cullen JJ, Sarr MG, Ilstrup DM. Pancreatic anastomotic leak after pancreaticoduodenectomy: incidence, significance, and management. Am J Surg 1994;168:295-8. [PubMed]
- Haddad LB, Scatton O, Randone B, et al. Pancreatic fistula after pancreaticoduodenectomy: the conservative treatment of choice. HPB (Oxford) 2009;11:203-9. [PubMed]
- Farley DR, Schwall G, Trede M. Completion pancreatectomy for surgical complications after pancreaticoduodenectomy. Br J Surg 1996;83:176-9. [PubMed]
- Vonlanthen R, Slankamenac K, Breitenstein S, et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg 2011;254:907-13. [PubMed]
- Čečka F, Jon B, Šubrt Z, et al. Clinical and economic consequences of pancreatic fistula after elective pancreatic resection. Hepatobiliary Pancreat Dis Int 2013;12:533-9. [PubMed]