Intrahepatic pseudoaneurysm after radiofrequency ablation of liver metastases
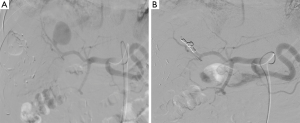
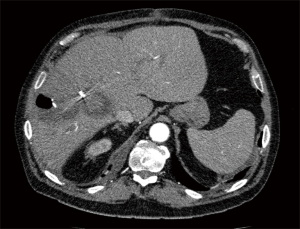
A 74-year-old man presented history of fever and abdominal pain 1 month following a simultaneous hepatic resection and 2 radiofrequency ablations (RFA) under ultrasound control for metachronous colonic liver metastases. Contrast-enhanced computed tomography (CT) showed a collection with an air-fluid level and a hypervascular enhancing lesion within the hypodense region of the RFA (Figure 1, arrow). An arteriography confirmed the diagnosis of pseudoaneurysm (Figure 2A).

What is your therapeutic strategy?
A transarterial selective embolisation with coils was successfully performed (Figure 2B). The postprocedural CT showed no evidence of filling of the aneurysm (Figure 3). The patient had an uneventful recovery. A 12-month follow-up CT scan of the liver showed postablation changes without evidence of recurrence of the aneurysm.
RFA is a spreading technique in the therapeutic armamentarium to treat liver lesions. Biliary stricture, hepatic abscesses, and portal thrombosis are the most procedure-specific complications. The occurrence of pseudoaneurysm is rare, with very few cases reported in the literature (1-3) but should be known and treated preferentially by endovascular approach to prevent a massive abdominal bleeding. Most cases can be managed by angioembolization. In our team, this is the first therapeutic option, assuming that expert angiography is readily available. However, in patients with failed embolization, emergency surgery could be required.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Datta RV. Intrahepatic pseudoaneurysm after radiofrequency ablation of liver lesion. Int Surg 2008;93:381-4. [PubMed]
- Tamai F, Furuse J, Maru Y, et al. Intrahepatic pseudoaneurysm: a complication following radio-frequency ablation therapy for hepatocellular carcinoma. Eur J Radiol 2002;44:40-3. [PubMed]
- Chuang CH, Chen CY, Tsai HM. Hepatic infarction and hepatic artery pseudoaneurysm with peritoneal bleeding after radiofrequency ablation for hepatoma. Clin Gastroenterol Hepatol 2005;3:A23. [PubMed]