
Clinical value and cost-effectiveness of minimally invasive distal pancreatectomy
Minimally invasive pancreatic resection (MIPR) has gained popularity in the last decade and it is currently widely applied with selected indications in highly specialized centres worldwide. Distal pancreatectomy (DP), which lacks of a technical demanding and complex reconstruction phase, is the most suitable pancreatic resection for a minimal invasive approach and is therefore the most performed MIPR. Several non-randomized studies and meta-analyses suggested that a minimally invasive distal pancreatectomy (MIDP) could improve the short-term postoperative outcomes by reducing the intraoperative blood loss and the postoperative morbidity when compared to open distal pancreatectomy (ODP) (1). MIDP seems also to promote an earlier recovery and a reduction in the length of postoperative stays when compared to ODP without affecting the oncologic outcomes. Therefore, the diffusion of MIDP is increasing and a minimally invasive approach is generally recognized as a suitable approach to benign, borderline malignant lesions and to Pan-NENs. The value of MIDP for the surgical treatment of pancreatic ductal adenocarcinoma (PDAC) is still under evaluation despite its feasibility and safety in this setting have been demonstrated and similar long-term oncological outcomes were reported by several single and multicentre series (2). The recent published DIPLOMA study, a European retrospective propensity score-matched cohort study on minimally invasive versus open DP for PDAC, raised some concerns in terms of oncological adequacy of MIDP (3). In fact, despite a similar reported overall survival between ODP and MIDP a lower lymph nodes retrieval and a lower incidence of Gerota’s fascia resection were observed in the MIDP group. Results of the LEOPARD trial, the first multicentre patient blinded randomized controlled trial comparing the outcomes of open versus MIDP (10% of minimally invasive case operated by robotic approach), showed a reduction of intra operative blood loss, delayed gastric emptying and a shorter postoperative hospital stay in the MIDP group (4). Mortality and major complications (Clavien-Dindo ≥3 were similar between groups. Surprisingly results of 1-year follow-up of the LEOPRAD trial highlighted a higher-grade B/C pancreatic fistula rate in the MIDP group (5). These concerning results have not been reported before and highlight the need for long-term follow-up to correctly assess not only the clinical impact of MIDP but also the quality of life and cumulative costs related to the procedure. It is therefore of paramount importance to assess late complications and readmission rates as well as the impact of a faster recovery after surgery can have on the quality of life of patients and to their return to an active working life (which also has an important effect on the social costs of a surgical procedure). Nowadays the economic and social costs of surgery have to be investigated in terms of both cost-utility and cost-effectiveness and have to be addressed from the perspective of different health care systems. Cost benefit analysis of a new surgical procedure such as MIDP should be considered a benchmark for the full implementation of new techniques since an effective allocation of the health care system economic resources is mandatory. Nevertheless, the cost-effectiveness of MIDP is still ill defined. Several studies were focused on costs comparison between open and laparoscopic DP (6-8) but few data are available on cost-effectiveness of robotic MIDP (r-MIDP), which carries in general higher operative room costs (both for materials and for length of operation related factors). Since now, only three studies addressed the comparative costs analysis of the open, laparoscopic and robotic DP (Table 1) (9-11). In general, as reported by Gavriilidis et al. robotic MIDP has been associated with a 1-day reduction in hospital stay when compared to laparoscopic MIDP (12). Whether, this benefit could balance the higher costs of r-MIDP related to surgical equipment and longer operative room time is unclear. An accurate assessment of the total costs supported by the health care system is difficult and generally biased by the different outcomes measured and discrepancy in long-term follow-up, as well as specific peculiarity of different health care systems. The recently published paper by Rodriguez et al. (9) is one of the few studies analysing the economic impact and the cost-effectiveness of different surgical approaches to DP. The authors reported a consecutive series of 89 patients submitted to DP at two French Institutions over a 4-year period. Patients were stratified by surgical approach: 21 were robotic (RDP), 25 laparoscopic (LDP), and 43 open (ODP). The robotic approach resulted to be associated with a lower intraoperative blood loss, an increase in splenic preservation rate and with a reduction in severe morbidity rate (Clavien-Dindo ≥ grade III). The robotic approach was associated to a longer operative time and a longer operative room costs. Interestingly, the costs of r-MIDP operation were counterbalanced by a reduction in postoperative stay and by a lower incidence of severe postoperative complications requiring extra treatment. Therefore, r-MIDP resulted to be the most cost-effective procedure even when compared to laparoscopy. In a deeper analysis of the results, it must be considered that the percentage of patients operated on for PDAC (patients at higher risk of morbidity and submitted for oncological reasons to an associated splenectomy) were highly different in the three groups (only 9.5% in the robotic group versus 32.5% and 51.1% in the laparoscopic and open group respectively). Nevertheless, the results reported by Rodriguez et al. suggest not only the clinical impact of the robotic approach but also the potentiality in terms of costs reduction of the robotic platform applied to MIDP.
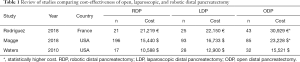
Full table
r-MIDP has still a limited diffusion and the most recent systematic review and network meta-analysis comparing open and MIDP (both laparoscopic and robotic) published in 2019 reported a still limited diffusion of the robotic approach which accounted for only 11% of the total sample (13). Advantages of the robotic platform are mainly related to magnified high-resolution 3D view and to the higher dexterity achievable with the robotic instruments thanks to seven degrees of freedom of the EndoWrist System. The robotic approach could also facilitate technically complex cases and has been reported to have an impact on the reduction of conversion rate to open surgery and to improve the rate splenic preservation (when appropriated). Robotic surgery seems also to facilitate and speed up the learning curve especially in surgeons not previously trained in laparoscopic surgery. Since an effective allocation of the health care system economic resources is mandatory, it is important to make an effort in addressing the subset of patients which can benefit the most from a MIDP (both in terms of clinical outcomes and cost-effectiveness) in order to allocate patients to different approaches. In the paper by Xourafas et al. (14) an effort has been made to identify subclass of patients which could benefit the most from a minimally invasive approach both in terms of clinical and economic impact. BMI >25, T stage ≥3 and ASA ≥3 resulted to be factors associated to a statistically significant reduction in costs after MIDP when compared to open resection. We believe that robotic MIPR will have a bright future thanks to upcoming technological developments and it will facilitate the training of minimally invasive complex procedures and promote a wider diffusion of MIDP. Nevertheless, an aspect to consider when dealing with cost-effectiveness analysis is the implementation of enhanced recovery after surgery (ERAS) protocols. In different settings the implementation of ERAS protocols has showed a significant reduction in hospital stay and total hospital cost which is more evident in patients operated on by a conventional open approach which tend to have postoperative outcomes more similar to those of the minimally invasive cases than to those of the laparotomic historical patients (15). Therefore, implementation of ERAS protocols could promote a faster recovery and led to a significant reduction of postoperative hospital stay even in patients operated by standard open approach. This could minimize the economic advantages associated to MIPS and should therefore be taken into account when dealing with an appropriate allocation of health care resources.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://hbsn.amegroups.org/article/view/10.21037/hbsn.2019.10.19/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the noncommercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-ncnd/4.0/.
References
- Venkat R, Edil BH, Schulick RD, et al. Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique: a systematic review and meta-analysis. Ann Surg 2012;255:1048-59. [Crossref] [PubMed]
- Kooby DA, Hawkins WG, Schmidt CM, et al. A multicenter analysis of distal pancreatectomy for adenocarcinoma: is laparoscopic resection appropriate? J Am Coll Surg 2010;210:779-85, 786-7. [Crossref] [PubMed]
- van Hilst J, de Rooij T, Klompmaker S, et al. Minimally Invasive versus Open Distal Pancreatectomy for Ductal Adenocarcinoma (DIPLOMA): A Pan-European Propensity Score Matched Study. Ann Surg 2019;269:10-7. [Crossref] [PubMed]
- de Rooij T, van Hilst J, van Santvoort H, et al. Minimally Invasive Versus Open Distal Pancreatectomy (LEOPARD): A Multicenter Patient-blinded Randomized Controlled Trial. Ann Surg 2019;269:2-9. [Crossref] [PubMed]
- van Hilst J, Strating EA, de Rooij T, et al. Costs and quality of life in a randomized trial comparing minimally invasive and open distal pancreatectomy (LEOPARD trial). Br J Surg 2019;106:910-21. [Crossref] [PubMed]
- Limongelli P, Vitiello C, Belli A, et al. Costs of laparoscopic and open liver and pancreatic resection: a systematic review. World J Gastroenterol 2014;20:17595-602. [Crossref] [PubMed]
- Limongelli P, Belli A, Russo G, et al. Laparoscopic and open surgical treatment of left-sided pancreatic lesions: clinical outcomes and cost-effectiveness analysis. Surg Endosc 2012;26:1830-6. [Crossref] [PubMed]
- Fisher AV, Fernandes-Taylor S, Schumacher JR, et al. Analysis of 90-day cost for open versus minimally invasive distal pancreatectomy. HPB (Oxford) 2019;21:60-6. [Crossref] [PubMed]
- Rodriguez M, Memeo R, Leon P, et al. Which method of distal pancreatectomy is cost-effective among open, laparoscopic, or robotic surgery? Hepatobiliary Surg Nutr 2018;7:345-52. [Crossref] [PubMed]
- Magge DR, Zenati MS, Hamad A, et al. Comprehensive comparative analysis of cost-effectiveness and perioperative outcomes between open, laparoscopic, and robotic distal pancreatectomy. HPB (Oxford) 2018;20:1172-80. [Crossref] [PubMed]
- Waters JA, Canal DF, Wiebke EA, et al. Robotic distal pancreatectomy: cost effective? Surgery 2010;148:814-23. [Crossref] [PubMed]
- Gavriilidis P, Lim C, Menahem B, et al. Robotic versus laparoscopic distal pancreatectomy - The first meta-analysis. HPB (Oxford) 2016;18:567-74. [Crossref] [PubMed]
- Gavriilidis P, Roberts KJ, Sutcliffe RP. Comparison of robotic vs laparoscopic vs open distal pancreatectomy. A systematic review and network meta-analysis. HPB (Oxford) 2019;21:1268-76. [Crossref] [PubMed]
- Xourafas D, Cloyd JM, Clancy TE, et al. Identifying Hospital Cost Savings Opportunities by Optimizing Surgical Approach for Distal Pancreatectomy. J Gastrointest Surg 2019;23:1172-9. [Crossref] [PubMed]
- Ratti F, Cipriani F, Reineke R, et al. Impact of ERAS approach and minimally-invasive techniques on outcome of patients undergoing liver surgery for hepatocellular carcinoma. Dig Liver Dis 2016;48:1243-8. [Crossref] [PubMed]


