Surgical treatment of primary hepatocellular carcinoma with intrapericardial tumor thrombus without extracorporeal circulation
Malignant liver tumor is known for its tendency towards metastasis and vascular invasion. In patients with primary hepatocellular carcinoma (HCC), tumor thrombus (TT) in the portal vein is frequently encountered, and invasion of the hepatic vein has comparatively lower incidence (1). TT extension in the inferior vena cava (IVC) and right atrium (RA) is rarely observed and is always accompanied with tumor cell infiltration in the peripheral blood (2).
Inferior vena cava tumor thrombus (IVCTT) in malignant liver tumor is classified into three categories according to the thrombus location: (I) infradiaphragmatic type, (II) intrapericardial type, and (III) right atrium (RA) type (3). Patients diagnosed with IVCTT are mostly defined in the advanced stage and have relatively poor prognosis as the result of metastasis, TT shedding, or hemodynamic disorder. Surgical indications (BCLC, NCCN, JIS, CUPI) recommend patients beyond C stage (Barcelona Clinic Liver Cancer Staging) of primary HCC with IVCTT and without metastasis to receive palliative operation. In the past few decades, surgical treatment was not extensively applied to patients with IVCTT because of unexpected risks such as pulmonary embolism or pericardial tamponade by TT shedding during the operation procedure. Also, operations in type 3 IVCTT were generally performed through deep hypothermia and circulatory arrest (DHCA), which could lead to potential complications such as hypoxic edema of the nervous system and severe acidosis. In addition, patients with hepatocirrhosis always suffered from coagulation dysfunctions. Consequently, these patients were more susceptible to secondary bleeding after operation due to the utilization of heparin during extracorporeal circulation. Furthermore, life quality and survival time changes by surgical treatments were not distinct (4). However, non-operation treatment such as chemotherapy was inefficient for symptom remission or risk reduction. Both transcatheter arterial chemoembolization (TACE) and stereotactic radiotherapy demonstrate partial response to IVCTT control (5). Therefore, a precise and valid treatment discipline for malignant liver tumor with IVCTT still needs to be defined.
Recently, a clinical study demonstrated a prolonged average survival period in patients with primary HCC and IVCTT through surgical removal of both the tumor and thrombus (6). This study consisted of 25 cases of surgical treatments, 20 cases of chemoembolization treatments, and 11 cases with symptomatic treatment only. All patients within this study were potential candidates for surgery. Patients who were finally treated with an operation had a median survival of 19 months. Patients in the non-operation group had a median survival around 4–5 months. The theory of prolonged survival time by surgical treatment relied on the risk reduction of thrombus shredding and systemic metastasis. This clinical outcome provides support for electing surgical treatment in the patient who has resectable primary tumor with IVCTT and sufficient hepatic reservoir, and indicates that a significant improvement of patient survival by operation is possible.
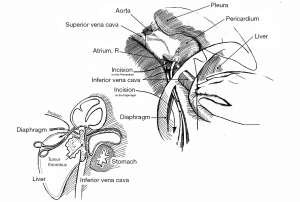
In addition, the surgical procedures in cases with supradiaphragmatic type IVCTT, especially intrapericardial type IVCTT, have been modified for patient benefit. Former operations for supradiaphragmatic IVCTT frequently performed median sternotomy, mediastinotomy, and pericardiectomy in order to clamp the IVC selectively above the TT. However, these approaches trigger unavoidable surgical trauma and increase the risk of severe postoperative complications such as pericardial tamponade (7). Thus, a new operation approach for embolectomy of intrapericardial type IVCTT has been proposed to reduce the potential risk of surgery.
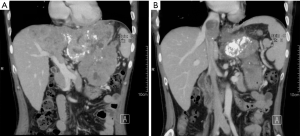
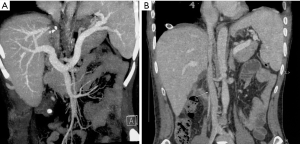
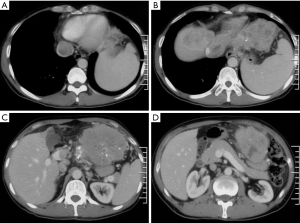
Dr. Lu’s team (Department of Liver Surgery, Peking Union Medical College Hospital) has performed 5 cases of operations on patients with malignant liver tumors and intrapericardial type IVCTT through a new surgical approach that does not use median sternotomy. One typical case was a 41-year-old male with severe symptoms of abdominal distension and pain for months. Computed tomography (CT) indicated a massive left upper abdominal tumor from the liver with a left portal and intrapericardial TT extension (Figures 1,2). The patient had a strong desire to relieve symptoms and his tumor staging matched the operation significance of clinical guidelines (BCLC, NCCN, JIS, CUPI). The operation was conducted through the new surgical approach. First, the thrombus was removed in the left portal vein, and the left portal vein and hepatic artery were oversewn; then, the liver was split, and the left liver with tumor was cleft out with hepatic vein preservation; next, exposure of the right diaphragm via diaphragm incision through the right side of the IVC hiatus (esophagus located on the left side of IVC hiatus), pericardiotomy, and exposure of the RA (performed via total hepatic vascular occlusion and RA occlusion beyond the level of the thrombus) (Figure 3) were completed. Finally, the hepatic vein was cleft and the entire thrombus was removed. All procedures of thrombectomy were performed through the abdominal cavity with transesophageal echocardiography. The solid thrombus was removed as a whole and no symptom of acute pulmonary embolism was observed during the process. Significant symptom remission manifested post operation. CT demonstrated rectification in both IVC and hepatic venous reflux (Figure 4). Survival time change still needs to be recorded through long-term follow-up.
This approach demonstrated that IVCTT extending to the IVC at the intrapericardial level below the RA can be resected through the abdominal cavity under total hepatic vascular exclusion, without median sternotomy and cardio-pulmonary bypass (7). Therefore, patients with intrapericardial type IVCTT can benefit from this new approach by reducing the operation risk.
In summary, surgical treatments of malignant liver tumors with intracaval extension have demonstrated contributions to patients’ symptom remission and risk reduction of systemic metastasis. With precise, radiological diagnosis, operations without DHCA for intrapericardial type IVCTT are clinically efficient for the minimization of surgical trauma and avoidance of DHCA-related complications.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kanematsu M, Imaeda T, Minowa H, et al. Hepatocellular carcinoma with tumor thrombus in the inferior vena cava and right atrium. Abdom Imaging 1994;19:313-6. [Crossref] [PubMed]
- Lee IJ, Chung JW, Kim HC, et al. Extrahepatic collateral artery supply to the tumor thrombi of hepatocellular carcinoma invading inferior vena cava: the prevalence and determinant factors. J Vasc Interv Radiol 2009;20:22-9. [Crossref] [PubMed]
- Mulholland MW, Albo D, Dalman R, Hawn M, Hughes S, Sabel MS. Operative Techniques in Surgery.
- Wakayama K, Kamiyama T, Yokoo H, et al. Surgical management of hepatocellular carcinoma with tumor thrombi in the inferior vena cava or right atrium. World J Surg Oncol 2013;11:259. [Crossref] [PubMed]
- Matsuo Y, Yoshida K, Nishimura H, et al. Efficacy of stereotactic body radiotherapy for hepatocellular carcinoma with portal vein tumor thrombosis/inferior vena cava tumor thrombosis: evaluation by comparison with conventional three-dimensional conformal radiotherapy. J Radiat Res 2016;57:512-23. [Crossref] [PubMed]
- Wang Y, Yuan L, Ge RL, et al. Survival Benefit of Surgical Treatment for Hepatocellular Carcinoma with Inferior Vena Cava/Right Atrium Tumor Thrombus: Results of a Retrospective Cohort Study. Ann Surg Oncol 2013;20:914-22. [Crossref] [PubMed]
- Miyazaki M, Ito H, Nakagawa K, et al. An approach to intrapericardial inferior vena cava through the abdominal cavity, without median sternotomy, for total hepatic vascular exclusion. Hepatogastroenterology 2001;48:1443-6. [PubMed]