
Fatal graft versus host hemolytic reaction from Rhesus compatible mismatched liver transplantation
Matching for Rhesus (Rh) blood group is not part of organ allocation systems. The principle concern expressed in the literature is that Rh-negative recipients might become sensitized and produce anti-D antibody which would have consequences for them if transfusion with Rh-positive blood or a pregnancy were to occur later. While Rh allosensitization is thought to occur in over 80% of Rh-negative recipients of Rh-positive blood, Starzl reported that it is less much less common in organ (liver, heart, lung) recipients even if they received Rh-positive blood during the operation (1). A more recent review of pediatric liver transplantation confirms the very low rate of allosensitization of Rh recipients of grafts from Rh-positive donors (2). In theory, there should be no risk of rejection if the combination is reversed—Rh-negative donor to a Rh-positive recipient. Therefore, it does not appear to be necessary to consider Rh status when allocating organs for transplantation.
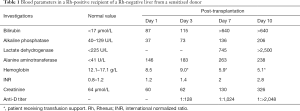
Recently we performed an ABO identical liver transplantation on a 60-year old Caucasian male with decompensated cirrhosis from non-alcoholic steatohepatitis. The patient was blood group A Rh-positive with a Model for End-stage Liver Disease score of 28. The donor was a 74-year-old female whose blood group was A Rh-negative. Rh sensitization was not considered at the time of transplantation but was found to be present retrospectively. The recipient had severe coagulopathy before the operation but the liver transplantation proceeded without incident requiring an intraoperative transfusion of packed red blood cells (5 units), cryoprecipitate (2 units) and platelets (4 units). On 4th post-operative day, he developed jaundice acutely and his hemoglobin dropped (Table 1). He was taken back to the operating room fearing an acute graft problem. The emergency laparotomy did not reveal any bleeding and the liver was in good condition. Therefore, hemolysis was considered and confirmed initially by a climbing lactate dehydrogenase. The direct antiglobulin (Coombs) test was positive whereas it was negative on historic pre-transplant blood. The cause was found to be anti-D antibody. The recipient was confirmed to be Rh-positive. Blood transfusion with Rh-negative blood, plasmapheresis and rituximab treatments were arranged. Immunosuppression was reduced. Anti-D antibody levels continued to increase dramatically (Table 1). The patient's condition deteriorated with the onset of renal failure and coma. He was unable to tolerate plasmapheresis or to consider ablative therapy with alemtuzumab (Campath 1H). Palliative measures were requested by his family and the patient died on the 10th post-operative day. Autopsy findings were compatible with advanced hemolytic disease. There was no evidence of intra-abdominal hemorrhage and all the liver anastomoses were patent and intact.
Full table
Passenger lymphocyte syndrome (PLS) was predicted and then described in the early days of organ transplantation (3). It is most common with ABO compatible mismatch (also called minor incompatibility), where immune hemolysis appears to be relatively benign, of limited duration (usually 6 weeks) and amenable to transfusion support using the donor’s type (antigen negative) blood. Reports of immune hemolysis related to Rh mismatched transplantation with a Rh allosensitized donor are much less common. Overall these reports are of more severe and persistent hemolysis than that seen with ABO minor incompatibility (3,4). In our patient, the production of antibody by the passenger lymphocyte clone was unrelenting causing severe hemolysis and its complications. We presume the Rh-negative female donor was sensitized during childbirth. We were able to determine that she had children between the ages of 20 and 35, the last being 40 years before her own death. Rh allosensitization is known to be lifelong despite an absence of the alloantigen. We previously reported a similarly persistent antibody against the platelet antigen HPA-1a, which caused life threatening thrombocytopenia in 3 recipients of the kidneys and liver, from a female HPA-1a negative donor, who had been sensitized during childbirth at least 20 years before organ donation (5). Only the liver was accepted for donation in the current report because of the donor’s age but we can presume that Rh-positive recipients of other organs, had they been transplanted, would also have been at risk of immune hemolysis.
Supportive care using antigen negative transfusion is often all that is required for ABO minor incompatibility. It was inadequate in our patient as it was in several of the previously reported Rh PLS cases (3,4). We reduced immunosuppression hoping the passenger clone from the donor would be rejected if the recipient's immune response was restored. This phenomenon with resolution of PLS has been reported before but does not occur reliably (4,5). Early aggressive intervention has been advised to eliminate the clone or reduce its capacity to produce antibody (3). We believe the time for such an intervention in our patient would have been before the 4th post-operative day. Monitoring of anti-D antibody titer is required at least daily. If it is rising early consideration should be given to lymphocyte ablation with alemtuzumab or a similar agent
In the end, the best strategy will be to avoid the situation altogether. This requires us to test all Rh-negative donors for sensitization. If anti-D antibody is found in a donor, the organs should be allocated to Rh-negative candidates for transplantation. It has been estimated that a Rh minor incompatible match with a sensitized Rh-negative donor should occur only 3 times per 1,000 transplantations (4) and therefore the requirement for Rh identical matching in this situation would be a reasonable precaution.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ramsey G, Hahn LF, Cornell FW, et al. Low rate of Rhesus immunization from Rh-incompatible blood transfusions during liver and heart transplant surgery. Transplantation 1989;47:993-5. [Crossref] [PubMed]
- Bolia R, Shankar S, Herd L, Hardikar W. Rhesus Alloimunization Occurs After Rh Incompatible Liver Transplantation in Children. Transplantation 2018;102:e1. [Crossref] [PubMed]
- Cserti-Gazdewich CM, Waddell TK, Singer LG, et al. Passenger lymphocyte syndrome with or without immune hemolytic anemia in all Rh-positive recipients of lungs from rhesus alloimmunized donors: three new cases and a review of the literature. Transfus Med Rev 2009;23:134-45. [Crossref] [PubMed]
- Gniadek TJ, McGonigle AM, Shirey RS, et al. A rare, potentially life-threatening presentation of passenger lymphocyte syndrome. Transfusion 2017;57:1262-6. [Crossref] [PubMed]
- West KA, Anderson DR, McAlister VC, et al. Alloimmune thrombocytopenia after organ transplantation. N Engl J Med 1999;341:1504-7. [Crossref] [PubMed]


