
Surgical treatment of ovarian cancer liver metastasis
Introduction
Recently, surgical indications for metastatic liver cancer (MLC) are gradually expanded. For instance, in the patients with colorectal cancer liver metastasis (CRLM), 5-year overall survival (OS) of these patients is more than 50% after receiving radical resection and standard postoperative treatments (1-3). Minimally invasive, laparoscopic liver resection (LR) can also benefit the CRLM patients (4). In addition, neuroendocrine cancer liver metastasis (NCLM) has also achieved satisfactory results, 5-year OS of which is 60–80% (5). Except for the CRLM and NCLM, the postoperative prognosis of patients with liver metastases from genital system tumor is significantly better than that from non-genital system tumor (6).
In the female genital system tumor, 75% of ovarian cancer (OC) patients are in the advanced-stage and 12–33% of which are in the stage IV at the initial diagnosis due to insidious progress (7,8). Since the 1970s, gynecologists were aware of the value of cytoreductive surgery (CRS) for advanced OC (9). In recent years, the results from several meta-analysis indicated that every 10% R0 CRS increases the survival rate of OC patients by 5.5% (10). With the development of surgical techniques and oncological views, R0 CRS is a constantly modified concept. In 1970s, the most common definition of maximal CRS was that the maximal diameter of residual focus is ≤2 cm. Till now, R0 is considered as the target of CRS, the definition of which is no visible residual focus after CRS. After R0 CRS, 5-year OS can achieve 68 months. While 5-year OS will fall to 40 and 33 months in patients with ≤1 or >1 cm residual focus (11). Unfortunately, 5-year OS of patients is still less than 20%. Residual focus after CRS and chemotherapeutic resistance are two main factors deteriorating the prognosis (12).
Liver is one of the most common distant metastasis target organs of OC (7). A retrospective study from Deng et al. showed that in 1,481 patients, 37.49% of patients occurred liver metastasis (LM), which was the most common distant organ metastasis, followed by lymph node, lung, bone, and brain metastasis. The occurrence of LM was positively correlated with the OS of patients (13). The incidence of LM and the number of lesions would increase gradually as the tumor progressed. LM was verified in 48% of patients at their death and the number of metastatic lesions indicated poor prognosis (14,15).
There are great progresses in the hepatic surgery in these years, especially in treating non-hepatitis B or non-cirrhosis MLC. Because of the fierce progress and poor prognosis of OCLM, hepatic surgeons are responsible for assisting gynecologists to improve the prognosis of these patients by different perspectives and emphases from gynecologist. Therefore, it is necessary to discuss OCLM from the perspective of hepatic surgeons by literature review and to guide further research and clinical decision.
LR for ovarian cancer liver metastasis (OCLM)
LR for OCLM was first reported in 1963 (16). Subsequently, the researches focusing on the value of this treatment increased gradually, all the results of which demonstrated that LR is a safe and effective treatment and improves the prognosis of OCLM patients (17-19). R0 resection is necessary for treating OCLM. The OS of patients who received R0 LR and CRS were 50.1 months, which were significantly higher than that of patients who received R0 CRS and non-R0 LR (20.0 months) (10). Moreover, LR did not prolong the waiting time for chemotherapy after OCLM, which had adverse effects on the prognosis (20). However, even if the patients with unresectable LM receiving standard chemotherapy and other adjuvant treatments, OS are only about 10 months. Generally, the patients who were suitable for LR were highly selected. The selection criteria were relatively low systemic tumor burden, metastasis sites located in superficial sites, and limited size of tumors. Gynecologists were very cautious on LR. Therefore, multiple LMs with a depth of more than 1 cm were commonly evaluated as unresectable status (21). So, hepatic surgeons were responsible for LR.
OCLM pattern
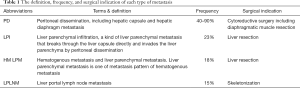
The most common metastasis patterns of OCLM are peritoneal dissemination (PD), hematogenous metastasis (HM) and lymph node metastasis (LNM) (22). PD is the most common pattern, corresponding to hepatic capsule and hepatic diaphragm metastasis, indicating OC stage III, which represents regional dissemination. PD can be found in the early stage of OC, and the number of disseminated foci is amazing, most of which are miliary nodules. In addition, PD can also cause liver parenchymal infiltration (LPI).
In the past, gynecologists paid great attention to the lesions of the hypogastrium, and the imaging examination and diagnosis of OCLM by PET-CT were not accurate enough. The actual incidence of HM may be higher than that have been known, corresponding to liver parenchymal metastasis (LPM), indicating OC stage IV, which represents extensive dissemination. Recently, the studies focusing on hepatic surgery related LNM [corresponding to liver portal LNM (LPLNM)] is not relatively rare (Table 1).
Full table
Miliary nodules dissemination between the right hemidiaphragm and liver capsule
Gynecologists generally use ultrasound examination to evaluate the lesions in upper abdomen, as a supplement for PET-CT. From the view of hepatic surgeons, the patients with advanced OC should be routinely performed an upper abdominal MRI to evaluate the metastases. The study from Patel et al. indicated that a certain proportion of patients with peritoneal carcinoma had LM, and vice versa (23). It is suggested that liver imaging can provide a reference for preoperative evaluation of PD. In addition to imaging evaluation, peritoneal carcinomatosis index (PCI) is also an important part of preoperative evaluation, and the most common index used to quantify peritoneal metastasis and determine the feasibility of CRS (24). PCI >11 indicates the patients have poor prognosis, while the patients with PCI 0–5 will has a better prognosis than who with PCI 6–10. LR is more suitable for patients with lower PCI score (25). However, preoperative imaging diagnosis is still powerless for such diffuse metastases between the right hemidiaphragm and liver capsule. Thus, the intraoperative diagnosis in laparotomy is very important. R0 resection should not be difficult for miliary nodules by intraoperative inspection and palpation.
Non-miliary nodules between the right hemidiaphragm and liver capsule
Cancer cells float in ascites and circulate clockwise in the abdominal cavity by intestinal peristalsis and diaphragm movement (22). Therefore, the diaphragm (especially right hemidiaphragm surrounded liver), recessus hepatorenalis, and liver capsule are the predilection site of metastasis. For advanced or recurrent OC, the incidence of diaphragmatic metastasis was 20–40% (26,27), and it was even as high as 91% in some studies. According to the tumor infiltration depth, it could be divided into four types: diaphragmatic peritoneal, subperitoneal space, central tendon (muscular diaphragm) and pleural surface (28). There are much more often and extensive metastases on the right hemidiaphragm than that on the left hemidiaphragm, and what’s more, if metastases occur on the right hemidiaphragm, 80% of the patients will have a simultaneous tumor implantation on the left side (27). To the right hemi-diaphragmatic metastases, gynecologists prefer diaphragmatic peritoneal stripping rather than diaphragmatic tumor resection in order to reduce diaphragmatic injury and chest complications. However, it is impossible for a surgeon to determine whether the implanted tumors are adhesion or invasion of striated muscle from the naked eye. Thus, peritoneal stripping only may lead to tumor residual. If the tumor invasion is deep, blunt peritoneal stripping is much more difficult than diaphragmatic tumor resection, and the operation time and intraoperative bleeding are significantly increased. No thoracic metastasis occurred after resection of diaphragmatic tumor, and no significant increase in resection related complications, such as pleural effusion and infection (29). Diaphragmatic tumor resection contributes more R0 CRS. Hepatic surgeons are skilled in right hemidiaphragm dissection, liver mobilization, and diaphragm resection. It seems more proper for hepatic surgeons to treat right hemidiaphragm OC metastasis (30).
LPI
At present, no clear definition of LPI could be found in guidelines. Some studies defined that LPI is PD with at least 2 cm tumor invasion in the liver parenchyma (17). LPI accounted for about 23% of OCLM, and it is more often in older patients without R0 resection in the primary CRS. There was no significant difference in the prognosis of LPI patients receiving standard treatment compared with that of PD patients. Therefore, it is recommended that LPI should be treated according to stage III OC, and the resectability of LPI should be evaluated carefully (31).
Stages III vs. IV
The International Federation of Gynecology and Obstetrics (FIGO) defines perihepatic metastasis as stage III OC and LPM as stage IV OC (32) (Table 2). PD is the main OCLM pattern, which can be divided into three types: hepatic capsular metastasis, right hemidiaphragm metastasis, and LPI. The corresponding hepatic surgical treatment includes liver mobilization, hepatic capsular metastasis resection, partial diaphragm resection, and hepatic segmentectomy. R0 LR could benefit patients without increase in postoperative complications. For these disseminated and diffuse metastases, which is difficult in preoperative diagnose, non-R0 resection should not be accepted. Hepatic surgeons should explore the lesions very carefully during the operation for the best benefit of the patients.

Full table
The incidence of HM is much less than that of PD. However, it is in advanced stage of tumor, the value of liver surgery is not clear. Recent studies have shown that the incidence of LPM is 18%, the second largest cause of stage IV OC, which is only inferior to malignant pleural effusion (11). The patients with LPM show better prognosis than stage IVb OC patients with spleen, lung, brain, and other parenchymal organ metastases, especially in patients younger than 65 years old (31). Systemic chemotherapy shows a limited effect on LPM patients, and the median OS and progression free survival (PFS) of stage IV patients who only received chemotherapy were only 15 and 8 months respectively (33). In the 1990s, only 16% of LPM could be treated with R0 LR by gynecologists, while non-R0 LR did not improve prognosis (34). The patients receiving R0 LR have significantly better prognosis than that in patients receiving LPM biopsy only. The median OS of these two groups were 53 and 21 months, respectively (35). Although LPM is the most advanced-stage of OC, active and standard treatment, especially R0 LR, is still necessary.
Hepatic surgeons should not evaluate LPM as unresectable status easily. Many studies have gotten a similar result that there was no significant difference in prognosis between patients with stage IVb OC after receiving R0 LR and patients with stage IVa OC (36-38). Compared OCLM patients with PD origin and LPM origin after receiving R0 LR, there was no significant difference in prognosis (18). In addition, LPM patients undergoing R0 LR were associated with longer disease-free interval and fewer LPMs after LR indicated a better prognosis (39).
LPM with extrahepatic metastasis
For advanced-stage OC with LPM and extrahepatic metastasis, LR is important components of CRS. It could improve the prognosis as part of primary, secondary, tertiary, and even quaternary CRS (18). The prognosis after R0 CRS in LPM patients with extrahepatic metastasis was not significantly different from that in patients with only LPM. Whether extrahepatic metastasis exists or not will not affect the prognosis of OC patients with LPM after receiving R0 CRS combined with systemic chemotherapy. Thus, LR should not be excluded from advanced-stage OC with extrahepatic metastasis (35).
LPM is the most advanced-stage of OC, associated with extrahepatic metastasis. Even in platinum sensitive patients, the effect of chemotherapy on LPM is limited. Local hepatectomy and anatomic LR are the main surgical modalities for the deeply located LPM. Hepatic surgeons should actively assist gynecologists to achieve R0 LR in the patients with LPM.
Unresectable LPM
R0 LR can significantly improve the prognosis of LPM patients and non-R0 LR cannot do that (19). Roh’s study defined the unresectable LPM: extensive abdominal metastasis or bilateral liver lobes extensive metastasis. The prognosis of the patients with unresectable LPM was significantly deteriorated (10 vs. 38 months) (40). On the other hand, OCLM with massive ascites were also considered that would significantly increase the rate of unresectable LPM (19). R0 LR is of great significance in the treatment of LPM and can significantly improve the prognosis of patients.
LNM
LNM is another major pattern of OCLM and cardiophrenic angle and even more distal LNM is not rare (41). Till now, some studies focused on LPLNM (42-46). The incidence of LPLNM and its impact on the prognosis of OCLM are poorly understood. Preoperative CT could accurately assess LPLNM, the incidence of which was 15%. Ninety percent of LPLNM could be R0 resected. However, the anatomical structure of the hilar region is complex, which makes lymph node dissection difficult. Gynecologists prefer to treat hilar lymph nodes by postoperative chemotherapy and radiotherapy rather than surgical resection. LPLNM R0 resection is an important part of R0 CRS. Compared with postoperative complication rate of CRS (30%), no LPLNM resection-related complications such as arterial hemorrhage and bile leakage were found (47). LPLNM was present in 15% of advanced OC patients. Intraoperative palpation should be performed very carefully in spite of no LPLNM evidence in preoperative CT, especially in the OC patients with para-aortic, mesenteric, and lesser omental lymph node metastases. LPLNM was also an independent prognostic factor as well as tumor stage (48). Hepatic surgeons are familiar with hilar skeletonization and hepatic surgeons may be more suitable to evaluate the resectability of hilar lymph node than gynecologists. The prognosis of LPLNM is not optimistic, although it is not the latest stage of OC. Hilar lymph node dissection and skeletonization are the main treatment methods. Intraoperative examination of hepatic hilar region should be emphasized, especially in the patients with other celiac lymph node metastases. Meanwhile, liver surgery should be carefully operated to avoid injury of blood vessels and bile duct.
In summary, combined with literature review and our clinical experience, OCLM surgery may be recommended as follow:
- Open surgery may be more suitable than laparoscopic surgery. The middle abdominal incision from the xiphoid to the symphysis pubis.
- Gynecologists or gynecologic oncologists evaluate the possibility of extrahepatic R0 CRS. LR should be selected carefully if the possibility of extrahepatic focus residue is high.
- The possibility of R0 LM should be evaluated preoperatively and intraoperatively by a hepatic surgeon. Careful evaluation before the operation of advanced OC is necessary. In addition to PET-CT, routine upper abdominal MRI or CT instead of ultrasound is recommended. If it is necessary, MRCP could be chosen for the patients with hepatic portal metastasis. For unresectable OCLM, the application of associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) has not been reported. The experience should be accumulated. Even experienced gynecologic oncologists should be recommended receiving intraoperative consultation from hepatic surgeons.
- Liver wedge resection or at least 1cm cautery depth is recommended for hepatic capsule metastasis, not just resecting the lesions on the hepatic capsule surface.
- Diaphragmatic resection and repair instead of diaphragmatic peritoneal dissection after adequate liver mobilization should be recommended for the metastasis between the right hemidiaphragm and liver capsule.
- The patients with LPI should be treated follow the same treatment principles as the patients with LPM, and liver local or anatomical resection should be performed, and the resection margin could be considered more than 2 cm.
- For patients with LPLNM, hepatic portal skeletonization should be performed, rather than portal lymph node dissection.
R0 CRS is the most favorable determinant for the prognosis of OC patients, and R0 LR is a component of R0 CRS. Patients with advanced OC are often accompanied by massive ascites due to tumor peritoneal spread, but their liver function is generally tolerable to LR. Different surgical treatments for different OCLM patterns, the common principle is to achieve R0 resection.
Non-surgical treatment
Radiofrequency ablation (RFA) provides an effective complement to hepatic surgery in OCLM patients with deep foci location and large tumor number. Till now, few numbers of cases reports showed the role of RFA in OCLM (49-51). RFA, as a local adjuvant therapy for OCLM, is feasible and effective. It provided great local tumor control and no postoperative complications such as bleeding, liver abscess, and bile leakage were observed. However, whether the therapeutic affection of RFA and LR are equal remain to be validated in large-scale sample prospective randomized controlled trials (52).
In addition to RFA, transcatheter arterial chemoembolization (TACE) is not the first-line treatment for MLC, but it is also a minimally invasive option in palliative treatment of OCLM. TACE (mitomycin + gemcitabine + cisplatin) was used for unresectable OCLM with poor response to systemic chemotherapy. The postoperative survival rates were 58%, 19%, and 13% at 1, 2, and 3 years, respectively. Compared with LR, TACE is a safe and effective palliative treatment option, because it is easy to operate and has fewer complications (53).
For the OCLM, Perioperative chemotherapy is still controversial. Regardless of pre- or postoperative adjuvant chemotherapy, the current first choice regimen is paclitaxel plus platinum and no regimen is especially for OCLM. In clinical practice, two to four courses of preoperative adjuvant chemotherapy may be advised. The advantages are tumor regression which is conducive to the operation and identifying primary drug resistance which accounts for about 20% of OC patients and indicates poor prognosis. However, there is no evidence to prove whether there is a clear correlation between the operation with or without preoperative chemotherapy and prognosis at present. Several RCT are undergoing to identify it.
The patients with BRCA mutation
Breast cancer patients with BRCA1/2 mutation had a high tendency of visceral metastasis, especially in lung and brain (54). It is suggested that the mutation of BRCA affects the metastasis pattern and increases the rate of visceral invasion. In OC, up to 92% of the patients with BRCA1/2 mutation had visceral metastasis. The liver, spleen, and lung metastasis were 42%, 32%, and 16%, respectively, significantly higher than 0%, 0%, and 3% in the control group (nonhereditary control patients from the Edinburgh Ovarian Cancer Database) (55).
The close correlation between BRCA mutation and visceral metastasis, especially LM, suggests that gene detection should also be performed for OCLM patients who deny family history. The gene detection could not only provide genetic counseling for patients and their families, but also identify whether the patients would be suitable for PARP inhibitor therapy. BRCA mutation involves not only platinum chemosensitivity, but also double-strand break defect. The results suggest that OC with BRCA mutation has unique clinical characteristics, which is also the basis of new molecular subtypes of OC with the different biological behavior and prognosis of tumors from that without BRCA mutation. After a comprehensive assessment, individualized treatment should be used more frequently, especially with BRCA1/2 mutation OCLM.
Summary
The studies focusing on MLC treated through hepatectomy is accumulating. R0 CRS can significantly improve the prognosis of OC, and surgical treatment of OCLM may be another hotspot except for CRLM. In despite of different OCLM modes, LR combined with adjuvant therapy are effective means, which can significantly improve the prognosis of OCLM with fewer complications. Individual treatment will provide more benefit to patients with BRCA mutations. Hepatic surgeons should cooperate with gynecologists to improve the prognosis of OCLM patients on the basis of R0 LR. Further basic research and large-scale samples prospective randomized controlled clinical trials are needed to clarify the molecular mechanism and treatment of OCLM.
Acknowledgements
Funding: This work was jointly supported by National Natural Science Foundation of China (No. 81874182, 81874056, 81372314, 81272393 and 81773266), the National Key Project of China (No. 2017ZX10203204-007-004), the Public Health Bureau Foundation of Shanghai (No. 201840019), the Research Talent Foundation of Fudan University Shanghai Cancer Center (No. YJRC1604), and Key Disciplines Group Construction Project of Pudong Health Bureau of Shanghai (No. PWZxq2017-13).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Disclaimer: The funders had no role in study, design, data collection and analysis, decision to publish, or preparation of this work.
References
- Nordlinger B, Sorbye H, Glimelius B, et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet 2008;371:1007-16. [Crossref] [PubMed]
- Tomlinson JS, Jarnagin WR, DeMatteo RP, et al. Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol 2007;25:4575-80. [Crossref] [PubMed]
- de Haas RJ, Wicherts DA, Andreani P, et al. Impact of expanding criteria for resectability of colorectal metastases on short- and long-term outcomes after hepatic resection. Ann Surg 2011;253:1069-79. [Crossref] [PubMed]
- Kazaryan AM, Marangos IP, Rosok BI, et al. Laparoscopic resection of colorectal liver metastases: surgical and long-term oncologic outcome. Ann Surg 2010;252:1005-12. [Crossref] [PubMed]
- Mayo SC, de Jong MC, Pulitano C, et al. Surgical management of hepatic neuroendocrine tumor metastasis: results from an international multi-institutional analysis. Ann Surg Oncol 2010;17:3129-36. [Crossref] [PubMed]
- Weitz J, Blumgart LH, Fong Y, et al. Partial hepatectomy for metastases from noncolorectal, nonneuroendocrine carcinoma. Ann Surg 2005;241:269-76. [Crossref] [PubMed]
- Cannistra SA. Cancer of the ovary. N Engl J Med 2004;351:2519-29. [Crossref] [PubMed]
- Prat J. FIGO Committee on Gynecologic Oncology. Abridged republication of FIGO's staging classification for cancer of the ovary, fallopian tube, and peritoneum. Cancer 2015;121:3452-4. [Crossref] [PubMed]
- Griffiths CT. Surgical resection of tumor bulk in the primary treatment of ovarian carcinoma. Natl Cancer Inst Monogr 1975;42:101-4. [PubMed]
- Bristow RE, Tomacruz RS, Armstrong DK, et al. Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J Clin Oncol 2002;20:1248-59. [Crossref] [PubMed]
- Winter WE 3rd, Maxwell GL, Tian C, et al. Tumor residual after surgical cytoreduction in prediction of clinical outcome in stage IV epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol 2008;26:83-9. [Crossref] [PubMed]
- Rauh-Hain JA, Rodriguez N, Growdon WB, et al. Primary debulking surgery versus neoadjuvant chemotherapy in stage IV ovarian cancer. Ann Surg Oncol 2012;19:959-65. [Crossref] [PubMed]
- Deng K, Yang C, Tan Q, et al. Sites of distant metastases and overall survival in ovarian cancer: A study of 1481 patients. Gynecol Oncol 2018;150:460-5. [Crossref] [PubMed]
- Rose PG, Piver MS, Tsukada Y, et al. Metastatic patterns in histologic variants of ovarian cancer. An autopsy study. Cancer 1989;64:1508-13. [Crossref] [PubMed]
- Aletti GD, Podratz KC, Cliby WA, et al. Stage IV ovarian cancer: disease site-specific rationale for postoperative treatment. Gynecol Oncol 2009;112:22-7. [Crossref] [PubMed]
- Brunschwig A. Hepatic lobectomy for metastatic cancer. Cancer 1963;16:277-82. [Crossref] [PubMed]
- Bacalbaşa N, Balescu I, Dima S, et al. Long-term Survivors After Liver Resection for Ovarian Cancer Liver Metastases. Anticancer Res 2015;35:6919-23. [PubMed]
- Bacalbasa N, Dima S, Brasoveanu V, et al. Liver resection for ovarian cancer liver metastases as part of cytoreductive surgery is safe and may bring survival benefit. World J Surg Oncol 2015;13:235. [Crossref] [PubMed]
- Neumann UP, Fotopoulou C, Schmeding M, et al. Clinical outcome of patients with advanced ovarian cancer after resection of liver metastases. Anticancer Res 2012;32:4517-21. [PubMed]
- Wright JD, Herzog TJ, Neugut AI, et al. Effect of radical cytoreductive surgery on omission and delay of chemotherapy for advanced-stage ovarian cancer. Obstet Gynecol 2012;120:871-81. [Crossref] [PubMed]
- Lim MC, Kang S, Lee KS, et al. The clinical significance of hepatic parenchymal metastasis in patients with primary epithelial ovarian cancer. Gynecol Oncol 2009;112:28-34. [Crossref] [PubMed]
- Nakayama K, Nakayama N, Katagiri H, et al. Mechanisms of ovarian cancer metastasis: biochemical pathways. Int J Mol Sci 2012;13:11705-17. [Crossref] [PubMed]
- Patel CM, Sahdev A, Reznek RH. CT. MRI and PET imaging in peritoneal malignancy. Cancer Imaging 2011;11:123-39. [Crossref] [PubMed]
- Jacquet P, Sugarbaker PH. Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. Cancer Treat Res 1996;82:359-74. [Crossref] [PubMed]
- Saxena A, Valle SJ, Liauw W, et al. Limited synchronous hepatic resection does not compromise peri-operative outcomes or survival after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J Surg Oncol 2017;115:417-24. [Crossref] [PubMed]
- Zivanovic O, Eisenhauer EL, Zhou Q, et al. The impact of bulky upper abdominal disease cephalad to the greater omentum on surgical outcome for stage IIIC epithelial ovarian, fallopian tube, and primary peritoneal cancer. Gynecol Oncol 2008;108:287-92. [Crossref] [PubMed]
- Eisenhauer EL, Chi DS. Liver mobilization and diaphragm peritonectomy/resection. Gynecol Oncol 2007;104:25-8. [Crossref] [PubMed]
- Einenkel J, Ott R, Handzel R, et al. Characteristics and management of diaphragm involvement in patients with primary advanced-stage ovarian, fallopian tube, or peritoneal cancer. Int J Gynecol Cancer 2009;19:1288-97. [Crossref] [PubMed]
- Tsolakidis D, Amant F, Van Gorp T, et al. Diaphragmatic surgery during primary debulking in 89 patients with stage IIIB-IV epithelial ovarian cancer. Gynecol Oncol 2010;116:489-96. [Crossref] [PubMed]
- Kato K, Katsuda T, Takeshima N. Cytoreduction of diaphragmatic metastasis from ovarian cancer with involvement of the liver using a ventral liver mobilization technique. Gynecol Oncol 2016;140:577-9. [Crossref] [PubMed]
- O'Neill AC, Somarouthu B, Tirumani SH, et al. Patterns and Prognostic Importance of Hepatic Involvement in Patients with Serous Ovarian Cancer: A Single-Institution Experience with 244 Patients. Radiology 2017;282:160-70. [Crossref] [PubMed]
- Prat J. FIGO Committee on Gynecologic Oncology. Staging Classification for Cancer of the Ovary, Fallopian Tube, and Peritoneum: Abridged Republication of Guidelines From the International Federation of Gynecology and Obstetrics (FIGO). Obstet Gynecol 2015;126:171-4. [Crossref] [PubMed]
- Harries M, Gore M. Part II: chemotherapy for epithelial ovarian cancer-treatment of recurrent disease. Lancet Oncol 2002;3:537-45. [Crossref] [PubMed]
- Bristow RE, Montz FJ, Lagasse LD, et al. Survival impact of surgical cytoreduction in stage IV epithelial ovarian cancer. Gynecol Oncol 1999;72:278-87. [Crossref] [PubMed]
- Kamel SI, de Jong MC, Schulick RD, et al. The role of liver-directed surgery in patients with hepatic metastasis from a gynecologic primary carcinoma. World J Surg 2011;35:1345-54. [Crossref] [PubMed]
- Rosendahl M, Hogdall CK, Mosgaard BJ. Restaging and Survival Analysis of 4036 Ovarian Cancer Patients According to the 2013 FIGO Classification for Ovarian, Fallopian Tube, and Primary Peritoneal Cancer. Int J Gynecol Cancer 2016;26:680-7. [Crossref] [PubMed]
- Ataseven B, Harter P, Grimm C, et al. The revised 2014 FIGO staging system for epithelial ovarian cancer: Is a subclassification into FIGO stage IVA and IVB justified? Gynecol Oncol 2016;142:243-7. [Crossref] [PubMed]
- Paik ES, Lee YY, Lee EJ, et al. Survival analysis of revised 2013 FIGO staging classification of epithelial ovarian cancer and comparison with previous FIGO staging classification. Obstet Gynecol Sci 2015;58:124-34. [Crossref] [PubMed]
- Niu GC, Shen CM, Cui W, et al. Hepatic Resection is Safe for Metachronous Hepatic Metastases from Ovarian Cancer. Cancer Biol Med 2012;9:182-7. [PubMed]
- Roh HJ, Kim DY, Joo WD, et al. Hepatic resection as part of secondary cytoreductive surgery for recurrent ovarian cancer involving the liver. Arch Gynecol Obstet 2011;284:1223-9. [Crossref] [PubMed]
- Cowan RA, Tseng J, Murthy V, et al. Feasibility, safety and clinical outcomes of cardiophrenic lymph node resection in advanced ovarian cancer. Gynecol Oncol 2017;147:262-6. [Crossref] [PubMed]
- Rodriguez N, Miller A, Richard SD, et al. Upper abdominal procedures in advanced stage ovarian or primary peritoneal carcinoma patients with minimal or no gross residual disease: an analysis of Gynecologic Oncology Group (GOG) 182. Gynecol Oncol 2013;130:487-92. [Crossref] [PubMed]
- Song YJ, Lim MC, Kang S, et al. Extended cytoreduction of tumor at the porta hepatis by an interdisciplinary team approach in patients with epithelial ovarian cancer. Gynecol Oncol 2011;121:253-7. [Crossref] [PubMed]
- Raspagliesi F, Ditto A, Martinelli F, et al. Advanced ovarian cancer: omental bursa, lesser omentum, celiac, portal and triad nodes spread as cause of inaccurate evaluation of residual tumor. Gynecol Oncol 2013;129:92-6. [Crossref] [PubMed]
- Martinez A, Pomel C, Mery E, et al. Celiac lymph node resection and porta hepatis disease resection in advanced or recurrent epithelial ovarian, fallopian tube, and primary peritoneal cancer. Gynecol Oncol 2011;121:258-63. [Crossref] [PubMed]
- Gallotta V, Fanfani F, Fagotti A, et al. Mesenteric lymph node involvement in advanced ovarian cancer patients undergoing rectosigmoid resection: prognostic role and clinical considerations. Ann Surg Oncol 2014;21:2369-75. [Crossref] [PubMed]
- Tozzi R, Traill Z, Garruto Campanile R, et al. Porta hepatis peritonectomy and hepato-celiac lymphadenectomy in patients with stage IIIC-IV ovarian cancer: Diagnostic pathway, surgical technique and outcomes. Gynecol Oncol 2016;143:35-9. [Crossref] [PubMed]
- Gallotta V, Ferrandina G, Vizzielli G, et al. Hepatoceliac Lymph Node Involvement in Advanced Ovarian Cancer Patients: Prognostic Role and Clinical Considerations. Ann Surg Oncol 2017;24:3413-21. [Crossref] [PubMed]
- Bojalian MO, Machado GR, Swensen R, et al. Radiofrequency ablation of liver metastasis from ovarian adenocarcinoma: case report and literature review. Gynecol Oncol 2004;93:557-60. [Crossref] [PubMed]
- Cirimbei C, Prunoiu V, Marincas M, et al. Chirurgia (Bucur) 2011;106:465-73. [Radiofrequency ablation for liver metastases--mini invasive therapeutic option for patients with unresecable tumors]. [PubMed]
- Bleicher RJ, Allegra DP, Nora DT, et al. Radiofrequency ablation in 447 complex unresectable liver tumors: lessons learned. Ann Surg Oncol 2003;10:52-8. [Crossref] [PubMed]
- Liu B, Huang G, Jiang C, et al. Ultrasound-Guided Percutaneous Radiofrequency Ablation of Liver Metastasis From Ovarian Cancer: A Single-Center Initial Experience. Int J Gynecol Cancer 2017;27:1261-7. [Crossref]
- Vogl TJ, Naguib NN, Lehnert T, et al. Initial experience with repetitive transarterial chemoembolization (TACE) as a third line treatment of ovarian cancer metastasis to the liver: indications, outcomes and role in patient's management. Gynecol Oncol 2012;124:225-9. [Crossref] [PubMed]
- Fasano J, Muggia F. Breast cancer arising in a BRCA-mutated background: therapeutic implications from an animal model and drug development. Ann Oncol 2009;20:609-14. [Crossref] [PubMed]
- Gourley C, Michie CO, Roxburgh P, et al. Increased incidence of visceral metastases in scottish patients with BRCA1/2-defective ovarian cancer: an extension of the ovarian BRCAness phenotype. J Clin Oncol 2010;28:2505-11. [Crossref] [PubMed]


