Laparoscopic liver resection: a review of current indications and surgical techniques
Introduction
Radical surgical resection is still one of the most important curative treatments for most liver masses. Attempts at managing diseases of hepato-biliary system through laparoscope was started in 1987, surgeons performed the first case of laparoscopic cholecystectomy (1). Ever since then, laparoscopic approach soon became a wide-adopted standard procedure for patients who need a cholecystectomy. However, as limitations of technique and defects of equipment still remained, it was 4 years later until the first attempt of laparoscopic liver resection (LLR) was made (2). Initial reports of LLR indicated that the outcomes of the patients were comparable to the traditional open approach, which led to positive conclusions that in selected patients, LLR can be a safe and effective treatment. Since then, LLR has become a potentially alternative to traditional open liver resection.
The initial development of LLR was slow, only sporadic cases with local resection were reported (3-6). Left lateral sectionectomy was first reported in 1996, which inspired the interests of surgeons on LLR although the first case was converted to open surgery because of intraoperative massive bleeding (7,8). Since then, with accumulated experience, the cases of LLR increased dramatically around the world, quickly expanding to laparoscopic hemi-hepatectomy, single segmentectomy (not limited to II or III), trisectionectomy (extended or limited anatomical resection), and living donor liver donation (9-11).
The first international experts’ consensus conference was held in 2008 to summarize and assess the feasibility and safety of the remarkable development (12). The concept of major liver resections was defined as hemi-hepatectomies, trisectionectomies and resections of the difficult posterior segments (IVa, VII, VIII). The conference affirmed that LLR was a safe and effective approach to the management of surgical liver disease in the hands well-trained surgeons with experience in hepatobiliary and laparoscopic surgery. On the other hand, it also listed the concerns of LLR abuse, including inappropriate widened indications and unstable clinical outcomes related to the lack of training standards and credentials. In 2015, the second conference updated consensus, evaluating the status of LLR with recommendations given (13), which mainly focused on the benefits, risks and techniques of LLR and provided references to its development. These two conferences, together with several retrospective studies, supported that LLR was not only not inferior to open procedure for both minor and major hepatic resections in terms of oncological outcomes, but also advantageous in many fields: less blood loss, decreased postoperative morbidity and shorter hospital stay (10,14-18). However, till now, limited conclusions from randomized controlled trials which have been called out worldwide were available, several concerns still remain controversial: what are the appropriate indications and contraindications? How should surgeons perform precise operations? Whether patients can really benefit from the laparoscopic approach and how?
In this review, we will discuss major concerns about LLR together with recent progress in this field which we hope can offer helps to LLR procedure reassessment and standardization.
Patients selection (open or laparoscopic)
As the barcelona clinic liver cancer (BCLC) staging system recommended, resection remains the first-line treatment for 0-A stage hepatocellular carcinoma (HCC) (19,20). For suitable patients selected for LLR, three important factors must be taken into account: the presence of cirrhosis, the location of the mass and the size of the mass. The importance of the latter two factors is different between benign and malignant disease. It is a generally accepted concept that for malignant disease, squeezing the lesion and a poor dissecting margin have a negative influence on long-term outcome. In the discussion below, we will focus mostly on LLR for malignant tumors.
Location of the tumor
Considering the poor exposure of the operation area and difficult bleeding control, it was challengeable to perform LLR for lesions in the posterosuperior part of the liver (21). The Louisville consensus noted that single, no larger than 5 cm lesions located in peripheral liver area (segment II to VI) would be an appropriate indication of LLR (12). As the skills and the experiences accumulated, resection of difficult segments (VII, VIII and IVa) and even caudal lobe was proved to be safe and repeatable. Dulucq et al. shared their experience of two isolated laparoscopic resections of the hepatic caudate lobe without eventful postoperative course (22). It is worth mentioning that there was a complication of inferior vena cava (IVC) injury in one case which made the procedure tough even though it did not lead to a conversion. Araki et al. proved the feasibility of the approach of caudate lobe resections by analyzing such cases around 14 years from 2000 to 2014 (23). Evidence from multicenter suggested that LLR for posterosuperior parts of the liver was feasible and safe (24-26).In addition, the authors pointed out that surgical techniques must be individualized according to the tumor location and its relationship to the major hepatic vessels. Zheng et al. summarized 281 patients who received LLR for lesions located posterosuperior liver segments (I, IVa, VII and VIII), in which the blood loss, complication rate, hospital stay and tumor recurrence was not significantly different comparing with anterolateral (II, III, IVb, V and VI) group, despite longer operation time, higher conversion rate and thinner resection margin (27). Until now, in the experienced centers, location of the tumor may not hamper the laparoscopic approach technically any more if the tumor is assessed resectable in conventional laparotomy.
Size of the tumor
It was well recognized that tumor size is a risk factor in both laparoscopic and open liver tumor resection. Invasion of the important structures which must be conserved in consideration of better inflow and outflow of remnant parenchyma by a large liver tumor is very common, for a LLR, exposing and retracting the tumor would necessarily increase the chance of tumor spread. To avoid the negative influence of the procedure, Louisville statement recommended that tumor measured more than 5 cm is not a good candidate for LLR. Interestingly, in recent years, several reports provided data on LLR for tumor more than 5 cm, the results of which implicated that tumor size may not be a negative risk factor for both short and long-term outcome.
Ai et al. conducted a single-center study to evaluate the outcomes of LLR for HCC with a tumor size of 5–10 cm (28). Ninety-seven of 275 included patients received LLR, the others received open procedure. The mean operative time, mean estimated intraoperative blood loss, and blood transfusion rate did not significantly differ. However, shorter postoperative hospital stay and lower postoperative complications were observed in LLR group. The outcomes from follow-up period (median overall follow-up time was 21 months and the median follow-up time of survivors was 23 months) showed no significant difference in tumor recurrence rate. The 1- and 3-year rates of overall survival (OS) time, as well as disease-free survival (DFS) rate, were also not significantly different between the two groups. And this gave positive evidence to response the worries of inadequate resection margin and unsatisfying radical resection rate in LLR for HCC. Another retrospective comparative study was performed between patients who underwent LLR for HCC of ≥5 and <5 cm (29). Outcomes indicated that the conversion rate, operation time, blood loss, postoperative hospital stay, the DFS and OS time (median follow-up time of 37 months) were comparable between the two groups.
Study about LLR for large intrahepatic cholangiocarcinoma (ICC) was also available. Besides the concerns similar to those of HCC (inadequate resection margin, tumor rupture, uncontrollable bleeding and tumor seeding), failure of lymph node dissection under laparoscopy was a problem that can not be neglected. Wei et al. analyzed perioperative and long-term outcomes in patients suffered from large (≥5 cm) or multiple (≥2 lesions) ICCs (30). The study drew a conclusion that compared with LLR for small ICCs, LLR for large lesions was technically safe, feasible, and oncologically effective in selected patients. Furthermore, comparisons with open liver resection for large or multiple were made in this study, and no evidence indicated that LLR was inferior in both short and long-term outcomes.
Malignant tumor larger than 10 cm seems no longer an absolute contraindication for LLR nowadays. A study about LLR for colorectal liver metastases showed LLR for tumors with diameter more than 10 cm is safe and effective, thus got the conclusion that tumor size of large colorectal liver metastases should not veto the selection of laparoscopic approach (31). Several LLR cases for huge benign lesion (>10 cm) were published recently (32-34). The procedures showed optimistic outcomes. However, the number of such cases is small and it may not be enough to prove LLR can be widely adopted in this series of patients. On the other hand, the increased operation time required in LLR for huge tumor may add extra risks, such as anesthetic accident, pulmonary infection and nursing problem. These potential problems may add extra worries on application of LLR in patients with big benign masses.
Laparoscopic living liver donation
In the field of living donor liver transplantation (include adult to child and adult to adult), LLR offers safe minimally invasive approach for donors. The report of the first laparoscopic living donor hepatectomy was published in 2002 (11). It was an adult to child case and the procedure was rapidly adopted by followers. Then laparoscopic left or right hepatectomies for adult to adult transplantation were performed (35,36). Laparoscopic living donor left lateral sectionectomy was proved to be safe and repeatable and had become a standard care in experienced centers (37). For the laparoscopic right liver donation, several reports have shown the feasibility of this procedure and it do have advantages in postoperative recovery and cosmetic demands (38,39). On the other hand, much more complicated operation and extremely strict donor screening criteria can not be ignored. Though there were successful cases reported, experts still regarded laparoscopic right donor hepatectomy as an immature technique and more data were required (40).
Cirrhosis
LLR for tumor complicated with underlying liver disease, mostly referring to liver cirrhosis, is controversial. Liver transplantation was regarded as a curative treatment for HCC patients with liver cirrhosis (41,42). Unfortunately, shortage of donor and high costs of the procedure made liver transplantation the last resort for these set of patients. Liver resection remains the first choice of treatment in most circumstances (19,20). The management of cirrhosis liver under laparoscope should be more patient and cautious because it is difficult to identify the important anatomic structures and the liver parenchyma’s weakened response to energy equipment. In early period, a number of reports affirmed the safety and feasibility of minor LLR for HCC in patients with cirrhosis (21,43-45). But it was documented that patients with HCC on cirrhotic liver might have a higher transfusion, conversion and complication rate (45). Aiming to further evaluate the procedure, study conducted by Belli et al. compared the outcomes between the laparoscopic and open groups in cirrhotic patients (46). Laparoscopic surgery had a lower morbidity rate than open surgery, and this might be related to LLR group had a smaller median tumor size than open group and LLR was less extensive. The 1- and 3-year OS rate was 94% and 67% respectively with the median OS of 63 months and the 1 and 3-year DFS rate was 78% and 53% respectively with the median DFS of 38 months. There was no significant difference in OS and DFS rates between laparoscopic and open groups. Similar studies showed LLR for HCC in cirrhotic liver could reduce severe complications and shorten hospital stay. Moreover, these studies offered 5-year OS and DFS rate (47,48). On the basis of similar surgical margin, there was a trend towards better OS rate in LLR group though the data had no statistically difference (70% in LLR group vs. 46% in open group). Studies on major LLR for cirrhosis liver were available recently. Yoon et al., Xu et al. provided data about major LLR for cirrhosis liver in their centers, respectively (49,50). Their studies may provide higher level evidence by using the propensity score-matched analysis (51). Contrasted with open procedure, LLR for cirrhosis liver required a longer operation time due to difficulty in dissecting liver parenchyma. The blood loss, postoperative complication rate, 2-year OS and DFS were comparable with the open group. All these evidences supported that LLR may be a viable alternative to open procedure even in patients with liver cirrhosis.
Surgical instruments and techniques
The development of LLR was closely related to the adoption of constantly updated surgical instruments (52,53). Generally, instruments can be classified as assistant decision-making parts and concrete operation parts.
Intraoperative ultrasonography (IOUS) and fluorescence imaging system
IOUS is not only useful but indispensable and it promoted the progress of LLR significantly (45,54-56). Several important decision-making parameters, the extent of tumors, relationship to blood vessels and the potential plane of resection can be clearly and readily displayed. as anatomical resection of malignant tumors had been proved with better long-term outcomes (57,58). In anatomical LLR, identification of the hepatic veins and Glissonian system is of vital importance in deciding the transection plane. Careful identification and management of the branches of these vessels with IOUS can minimize the risk of vascular injury. Another advantage is that IOUS is able to identify the omitted lesions and have significant influence on operation decision-making. The utilize of IOUS in LLR has been recommended in several guidelines (13,59,60).
However, the resection range in the cases of single anatomic segmentectomy can not be marked precisely simply by ultrasound alone. Intraoperative fluorescence imaging techniques using indocyanine green (ICG) is needed for identifying the boundary of segments by laparoscopic fluorescence imaging (61-63). By injecting ICG into the portal branch of target resection segments or adjacent segments after clamping segmental portal pedicle, a liver map of hyperfluorescence or hypofluorescence region appeared under a specific visual system (laparoscopic near-infrared camera system was chosen in the report). The method shared in the reports is considered to be a recommendation for standard anatomic LLR aiming to achieve a better oncological outcome. In the meanwhile, there were experiences indicating that the intraoperative fluorescence imaging techniques in LLR have a potential to provide diagnostic information for malignancy identification as a compensation of limited palpation (64).
Instruments in parenchyma transection
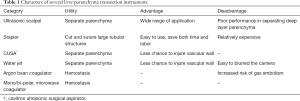
In terms of concrete operation, multitudinous innovative devices were used. in transecting the liver, there is not a conclusion on which device is superior to parenchymal transection yet (13,65).
Ultrasonic scalpel, stapler, cavitron ultrasonic surgical aspirator (CUSA) and water jet were mostly widely mentioned devices used to transect parenchyma while monopolar and bipolar cautery, argon beam coagulator, microwave coagulator were used to manage the cutting surface bleeding. By collecting data of 1499 LLR cases from 10 international centers, Buell et al. reported that parenchymal transection using stapler provides advantages of less blood loss and shorter operation time compared to electrosurgical resection (include radiofrequency ablation, tissuelink, ligasure and ultrasonic dissection) (66). However, resections using stapler provided a smaller pathological margin than the electrosurgical technique which leads to oncological concerns.
There was a review indicating that compared with CUSA and blunt dissection water jet had better performance in reducing blood loss and dissection time (67). But while using water jet in parenchymal dissection, camera would be often blurred by the device thus need frequent clean, make the process hard to proceed.
The efficiencies of bipolar compression devices and ultrasonic devices for LLR were evaluated in a retrospective control study (68). The bipolar compression devices were proved to have advantages in reducing transection time. In spite of the lack of significant difference in the estimated blood loss, bipolar compression devices had the tendency to provide better bleeding control. Ultrasonic devices utilized the vibration of its blades to cut and coagulate. Small vessels (≤3 mm) could be easily controlled by ultrasonic devices, bipolar compression devices, on the other hand, enabling the closing of vessels up to 7 mm in diameter (69-71). Moreover, the bipolar compression working principle allows gradual compressing and cauterizing the tissue followed by instant sealing and coagulation. Argon beam coagulator were introduced as an efficient transection plane hemostasis system. Whereas multi-center evidence demonstrated that argon bean coagulator increased the risk of gas embolism, its popularization was limited (13,72,73).
It is worth noting that the surgeons are required to have a comprehensive understanding of the advantages and limitations of their preference to ensure continually safe performance (65). A table of different liver parenchyma transection instruments shows their advantages and disadvantages (Table 1). A hand-assisted system was adopted to perform so-called hand-assisted LLR to reduce the degree of difficulty (74,75). With the accumulated experiences from practice, hand-assisted LLR was less frequently reported.
Full table
Position and approaches
A reverse Trendelenburg position with or without legs apart is commonly accepted worldwide (13,59). In this position, the blood flow returned to heart is reduced by gravity and the central venous pressure (CVP) is able to maintain in a low level (<5 cmH2O is recommended). In addition, the transverse colon, small intestine and omentum may keep a distance from the inferior surface of the liver, providing better view and larger operation space. The CO2 pneumoperitoneum pressure is generally set by 10–14 mmHg. For pure LLR, four, five or more trocars were inserted as needed. Usually a supra- or subumbilical incision was made as observation site, subcostal trocars were used as main operation ports. Most of LLRs are able to perform technically in this way. To handle the small lesions located in antero-superior or posterior part especially for segment VII and VIII, local or single segmentectomy may become a challenge due to a higher risk of insufficient surgical margin and difficult hemostasis. the repeatedly compression of liver tissue to mobilize and expose the lesion also increase the risk of tumor rupture and spread. Therefore, extended resections (resection of right posterior lobe even hemi-hepatectomy) are adopted in cases with the great loss of normal tissue. A novel method of semi-prone position was developed by a Japanese to provide a new visual (76,77). The patient was set in left lateral position with surgeons standing at the left side, after carefully fixed the operating table rotated by 20–25° to from semi-prone position. The utilization of this method increased LLR proportion for patients with lesions in antero-superior and posterior segments in their center (78). Fifty-six patients performed in semi-prone position were reviewed, compared to traditional supine position, this new approach was safe and showed benefits on reducing blood loss and hospital stay. Besides subcostal ports, an intercostal port is allowed to offer another direction to reduce lesion in hepatic dome. Just like the gravity works in reverse Trendelenburg position, the weight of the liver contributes to mobilization and right hepatic vein control. The posterior segment is positioned above IVC which may potentially reduce venous pressure. Chen et al. evaluated LLR with the jackknife position (79). The jackknife position, alike the semi-prone position, aims to deal with the lesions in segment VI, VII and VIII. However, poor exposure of the portal area makes inflow control difficult.
The difficulty of LLR varies with the range of resection. Besides partial hepatectomy in marginal area, laparoscopic left lateral section (LLLR) is considered as a simple and practicable method for beginners (80). Agreement was reached on considering LLLR as a standard of care in the first international conference (12). Although there has not been a procedure of precise standardized surgical technique for LLLR, laparoscopically stapled left lateral sectionectomy were commonly adopted in many centers as a result of minimizing blood loss and operation time (81-84). Two endoscopic liner staplers act as the key part of the procedure to separate pedicles of left lateral lobe and the left hepatic vein safely. Besides the two structures, there are seldom important large vessels or bile duct lied in the left side of the falciform ligament, which ensures a confident transection.
The major LLR is still a challenge through decades and should be performed only by experts (10,14). Mobilization of the right posterior segments, identification of intrahepatic anatomic variation, proficient of suture and ligation with laparoscopic apparatus as well as operation precisely and constantly for hours make the major LLR hard to master. The conventional approach of right liver resection needs mobilization of the right liver and control of right hepatic vein before transecting the parenchyma. For those large lesions located in right lobe of the liver, morphological disorder, surrounding structures adhesion and unstable tumor status make the conventional approach difficult to implement and the same is true in LLR. An anterior approach was introduced in the 1990s as an alternative to the conventional one. The method optimized the order of the procedure, putting parenchyma transection at first while mobilization in the end, and was frequently used in opening right hepatectomy as its various superiorities (85-87). Soubrane et al. conducted a similar caudal approach in LLR (13,88). The procedure started with intrafascial dissection of the right portal pedicle, the Cantlie line, the edge of IVC and the middle hepatic vein (MHV), which are important landmarks guiding the parenchyma resection. Unlike the conventional approach, MHV was firstly controlled, not until the resection reached the end could MHV be stapled. A retrospective comparative study, together with several case reports, verified the safety and feasibility of the caudal approach (89-92). Compared with the conventional approach, the caudal approach provides similar postoperative outcomes and benefits of reduced conversion rate.
In order to meet various situations, other novel approaches were also introduced. Yamashita et al. introduced a total transthoracic approach (93). In this case report, the patients previously received 3 major abdominal surgery. The transthoracic approach allowed the resection of liver tumor to perform smoothly by avoiding managing the great chaos in the abdominal cavity. A left-side approach was conducted by Cai et al. to provide convenience to anatomic caudal resection (94). The left-side approach had advantages especially for lesions arose from Spiegel’s lobe with or without spreading to right part of the caudate lobe, since most of these approaches were reported with limited cases, further studies are needed to prove their repeatability.
Massive blood loss and requirement of transfusion in liver resection have close relationship to the perioperative complications and malignancy recurrence (95,96). Bleeding control is one of the main concerns of all LLR. As previously discussed, LLR do have advantages in reducing blood loss and transfusion rate. An appropriate balance between pressure of CO2 pneumoperitoneum and CVP would be essential to decrease venous bleeding and maintain a stable hemodynamics (97). The pressure of pneumoperitoneum was commonly set as 10–14 mmHg and adjustment according to parameters of airway, CVP gradient was needed to reduce risks of gas embolism (98-100). In the meanwhile, surgeons must realize that meticulous hemostasis of transection plane is necessary because bleeding from small veins may stop temporarily by the effects of positive abdominal pressure. Low CVP (<5 cmH2O) is essential of bleeding control. Reverse Trendelenburg position, limited fluid infusion and short-term shutoff of mechanical ventilation in emergency offer helps.
Difficulty scoring/classifying system and learning curve of LLR
As previously mentioned, the difficulty of procedure varies greatly from type to type. A difficulty scoring or classifying system is necessary for preoperative preparation, especially for the beginners. Ban et al. came up with a difficulty scoring system based on several critical factors (resection extent, tumor size & location, proximity to important tubular structures and liver function). The system divided difficult index into three levels which gave guidance to surgeons (80). Although there were limitations, this novel difficulty system was widely adopted. Another similar difficulty classifying method presented by Kawaguchi simplified the evaluation steps (101). However, judging difficult levels merely based on operational related factors would not be able to meet the needs of precisely and individualized treatment. An international survey of potential factors which may add difficulty to operation from up to 80 experienced surgeons suggested that patient’s overall conditions should also be considered (102). These factors included BMI, history of chemotherapy, repeated liver resection and concurrent procedures. Hasegawa put forward a new model to predict surgical difficult of LLR. In this model obesity and platelet count were included.
For now, consensus had been reached that resection extent and lesion location were two main factors. left lateral sectionectomy and hemihepatectomy were regarded as two watersheds for the beginners, advanced learners and proficient. Unfortunately, none of the present difficult systems was fully satisfied. Thus, new ideas, which may at least include liver cirrhosis, were always welcome. On the other hand, another independent system—the learning curve may be useful for reference.
The learning curve describes the operation acquisition process of a settled team using cumulated sum or risk-adjusted cumulated sum analysis which regarding total operation time and total intraoperative blood loss as main observation indexes. According to literature reports, the learning curve of major hepatectomy was around 45 cases, the mean operation time was around 250–350 min and mean blood loss was around 300–500 mL (103-107). The result shows that surgeons may get stable outcomes after nearly 45 cases training under the premise of expertly performing open hepatectomy and simple LLR. As the LLR performed more and more worldwide, valuable experiences accumulated continuously. The learning curve of sophisticated LLR may become steeper which means that less cases are required. It is suggested that surgeons should start with wedge resection and do not take risk to try difficult LLR unless they can perform left lateral sectionectomy very well. Actually, mastering major LLR is a challengeable work indeed, recommendations are given that surgeons should perform major LLR with great cautiousness even though they have been quite familiar with laparoscopic surgery.
Robot hepatectomy
Robotic system is another minimally invasive approach which has been widely used in gastrointestinal, urinary and gynecological surgeries (108). It was applied for liver surgery in early 2010s, the initial experiences showed that robotic system can be used not only minor but also major liver resection (109,110). Recent reviews summarized the half-decade development of robotic liver surgery (111,112). Not limited to similar efficiency compared to conventional laparoscopic approach, its unique advantages of facilitating suturing under laparoscope allow it to provide more possibilities in the future. But on the other hand, a comparison conducted by Tsung showed that robot hepatectomy might not as perfect as we expected (113). What is more, higher cost of the robotic liver surgery probably makes it less appealing to patients, limited devices availability, relative fixed patient position and compromised assistant aiding would be also influence the choice of surgeons when confounding a difficult case.
Postoperative recovery
A concept of enhanced recovery after surgery (ERAS) was introduced by Kehlet in 1997 (114). ERAS is focused on optimizing perioperative management aiming to improve recovery, reduce postoperative morbidity and overall cost. The common strategies include preoperative education, individualized nutrition support, early oral intake and mobilization, appropriate analgesia etc. Achievements reached in many other surgical fields motivated ERAS to be applicated in liver surgery (115). A randomized control study, conducted to evaluate ERAS in LLR, verified these advantages (116). The patients underwent ERAS program benefited from lower morbidity rate, higher living quality and less cost. Among the various strategies, perioperative patient education, early postoperative mobilization, reduced drainage tubes, enhanced pain control, intravenous fluid restriction and oral nutrition played the essential part and also recommend by ERAS guideline for liver surgery (117).
Cost
The cost of treatment is a financial problem concerned by both medics and patients. LLR serves as a minimally invasive approach, kinds of high-tech laparoscopic equipment and instruments are indispensable and may increase the operation expense. However, surveys from multiple centers showed that, in most cases, total in-hospital cost of LLR was no higher than conventional open approach (118-121). This result probably related to shorter postoperative hospital stay and faster recovery when receive laparoscopic approach. Moreover, as the development of LLR goes faster, new low-cost techniques can be adopted without compromising surgical outcomes. And this gives an optimistic view of the future of LLR.
Conclusions
In conclusion, with the effort of both liver surgeons and medical engineers in recent two decades, LLR has become a technically practicable treatment for liver disease. Indications of LLR has expanded from local resection to difficult cases, even living donor allograft donation. with a learning curve of 45–60 cases, surgeons are able to perform continual high-quality operations of LLR (105). It was estimated that over 9,000 LLRs has been performed worldwide up to 2015, and the number is still in exponential growth. Even though few RCT is available at present, under the circumstance of quickly accumulated cases, many important questions regarding the oncological, cost-effective and technical aspects are about to get conclusions.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Litynski GS. Profiles in laparoscopy: Mouret, Dubois, and Perissat: the laparoscopic breakthrough in Europe (1987-1988). JSLS 1999;3:163-7. [PubMed]
- Reich H, McGlynn F, DeCaprio J, et al. Laparoscopic excision of benign liver lesions. Obstet Gynecol 1991;78:956-8. [PubMed]
- Katkhouda N, Fabiani P, Benizri E, et al. Laser resection of a liver hydatid cyst under videolaparoscopy. Br J Surg 1992;79:560-1. [Crossref] [PubMed]
- Klotz HP, Schlumpf R, Weder W, et al. Minimal invasive surgery for treatment of enlarged symptomatic liver cysts. Surg Laparosc Endosc 1993;3:351-3. [PubMed]
- Cunningham JD, Katz LB, Brower ST, et al. Laparoscopic resection of two liver hemangiomata. Surg Laparosc Endosc 1995;5:277-80. [PubMed]
- Hashizume M, Takenaka K, Yanaga K, et al. Laparoscopic hepatic resection for hepatocellular carcinoma. Surg Endosc 1995;9:1289-91. [Crossref] [PubMed]
- Azagra JS, Goergen M, Gilbart E, et al. Laparoscopic anatomical (hepatic) left lateral segmentectomy-technical aspects. Surg Endosc 1996;10:758-61. [Crossref] [PubMed]
- Kaneko H, Takagi S, Shiba T. Laparoscopic partial hepatectomy and left lateral segmentectomy: technique and results of a clinical series. Surgery 1996;120:468-75. [Crossref] [PubMed]
- Sasaki A, Nitta H, Otsuka K, et al. Ten-year experience of totally laparoscopic liver resection in a single institution. Br J Surg 2009;96:274-9. [Crossref] [PubMed]
- Dagher I, O'Rourke N, Geller DA, et al. Laparoscopic major hepatectomy: an evolution in standard of care. Ann Surg 2009;250:856-60. [Crossref] [PubMed]
- Cherqui D, Soubrane O, Husson E, et al. Laparoscopic living donor hepatectomy for liver transplantation in children. Lancet 2002;359:392-6. [Crossref] [PubMed]
- Buell JF, Cherqui D, Geller DA, et al. The International Position on Laparoscopic Liver Surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825-30. [Crossref] [PubMed]
- Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 2015;261:619-29. [PubMed]
- Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg 2009;250:831-41. [Crossref] [PubMed]
- Tranchart H, Dagher I. Laparoscopic liver resection: a review. J Visc Surg 2014;151:107-15. [Crossref] [PubMed]
- Cai XJ, Yang J, Yu H, et al. Clinical study of laparoscopic versus open hepatectomy for malignant liver tumors. Surg Endosc 2008;22:2350-6. [Crossref] [PubMed]
- Xu H, Liu F, Li H, et al. Outcomes following laparoscopic versus open major hepatectomy: a meta-analysis. Scand J Gastroenterol 2017;52:1307-14. [PubMed]
- Ciria R, Cherqui D, Geller DA, et al. Comparative Short-term Benefits of Laparoscopic Liver Resection: 9000 Cases and Climbing. Ann Surg 2016;263:761-77. [Crossref] [PubMed]
- Bruix J, Sherman M. Practice Guidelines Committee, et al. Management of hepatocellular carcinoma. Hepatology 2005;42:1208-36. [Crossref] [PubMed]
- Bruix J, Sherman M, Llovet JM, et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol 2001;35:421-30. [Crossref] [PubMed]
- Kaneko H, Takagi S, Otsuka Y, et al. Laparoscopic liver resection of hepatocellular carcinoma. Am J Surg 2005;189:190-4. [Crossref] [PubMed]
- Dulucq JL, Wintringer P, Stabilini C, et al. Isolated laparoscopic resection of the hepatic caudate lobe: surgical technique and a report of 2 cases. Surg Laparosc Endosc Percutan Tech 2006;16:32-5. [Crossref] [PubMed]
- Araki K, Fuks D, Nomi T, et al. Feasibility of laparoscopic liver resection for caudate lobe: technical strategy and comparative analysis with anteroinferior and posterosuperior segments. Surg Endosc 2016;30:4300-6. [Crossref] [PubMed]
- Cho JY, Han HS, Yoon YS, et al. Experiences of laparoscopic liver resection including lesions in the posterosuperior segments of the liver. Surg Endosc 2008;22:2344-9. [Crossref] [PubMed]
- Xiang L, Xiao L, Li J, et al. Safety and feasibility of laparoscopic hepatectomy for hepatocellular carcinoma in the posterosuperior liver segments. World J Surg 2015;39:1202-9. [Crossref] [PubMed]
- Teo JY, Kam JH, Chan CY, et al. Laparoscopic liver resection for posterosuperior and anterolateral lesions-a comparison experience in an Asian centre. Hepatobiliary Surg Nutr 2015;4:379-90. [PubMed]
- Zheng B, Zhao R, Li X, et al. Comparison of laparoscopic liver resection for lesions located in anterolateral and posterosuperior segments: a meta-analysis. Surg Endosc 2017;31:4641-8. [Crossref] [PubMed]
- Ai JH, Li JW, Chen J, et al. Feasibility and safety of laparoscopic liver resection for hepatocellular carcinoma with a tumor size of 5-10 cm. PLoS One 2013;8. [Crossref] [PubMed]
- Kwon Y, Han HS, Yoon YS, et al. Are large hepatocellular carcinomas still a contraindication for laparoscopic liver resection? J Laparoendosc Adv Surg Tech A 2015;25:98-102. [Crossref] [PubMed]
- Wei F, Lu C, Cai L, et al. Can laparoscopic liver resection provide a favorable option for patients with large or multiple intrahepatic cholangiocarcinomas? Surg Endosc 2017;31:3646-55. [Crossref] [PubMed]
- Nomi T, Fuks D, Louvet C, et al. Outcomes of Laparoscopic Liver Resection for Patients with Large Colorectal Liver Metastases: A Case-Matched Analysis. World J Surg 2016;40:1702-8. [Crossref] [PubMed]
- Kim SH, Kim KH, Kirchner VA, et al. Pure laparoscopic right hepatectomy for giant hemangioma using anterior approach. Surg Endosc 2017;31:2338-9. [Crossref] [PubMed]
- Wang S, Gao J, Yang M, et al. Intratumoral coagulation by radiofrequency ablation facilitated the laparoscopic resection of giant hepatic hemangioma: a surgical technique report of two cases. Oncotarget 2017;8:52006-11. [PubMed]
- van Rosmalen BV, Bieze M, Besselink MG, et al. Long-term outcomes of resection in patients with symptomatic benign liver tumours. HPB (Oxford) 2016;18:908-14. [Crossref] [PubMed]
- Samstein B, Cherqui D, Rotellar F, et al. Totally laparoscopic full left hepatectomy for living donor liver transplantation in adolescents and adults. Am J Transplant 2013;13:2462-6. [Crossref] [PubMed]
- Soubrane O, Perdigao Cotta F, Scatton O. Pure laparoscopic right hepatectomy in a living donor. Am J Transplant 2013;13:2467-71. [Crossref] [PubMed]
- Park JI, Kim KH, Lee SG. Laparoscopic living donor hepatectomy: a review of current status. J Hepatobiliary Pancreat Sci 2015;22:779-88. [Crossref] [PubMed]
- Suh KS, Hong SK, Lee KW, et al. Pure laparoscopic living donor hepatectomy: Focus on 55 donors undergoing right hepatectomy. Am J Transplant 2018;18:434-43. [Crossref] [PubMed]
- Takahara T, Wakabayashi G, Nitta H, et al. The First Comparative Study of the Perioperative Outcomes Between Pure Laparoscopic Donor Hepatectomy and Laparoscopy-Assisted Donor Hepatectomy in a Single Institution. Transplantation 2017;101:1628-36. [Crossref] [PubMed]
- Han HS, Cho JY, Kaneko H, et al. Expert Panel Statement on Laparoscopic Living Donor Hepatectomy. Dig Surg 2018;35:284-8. [Crossref] [PubMed]
- Llovet JM, Fuster J, Bruix J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology 1999;30:1434-40. [Crossref] [PubMed]
- Yao FY, Bass NM, Nikolai B, et al. Liver transplantation for hepatocellular carcinoma: analysis of survival according to the intention-to-treat principle and dropout from the waiting list. Liver Transpl 2002;8:873-83. [Crossref] [PubMed]
- Yamanaka N, Tanaka T, Tanaka W, et al. Laparoscopic partial hepatectomy. Hepatogastroenterology 1998;45:29-33. [PubMed]
- Cherqui D, Husson E, Hammoud R, et al. Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg 2000;232:753-62. [Crossref] [PubMed]
- Gigot JF, Glineur D, Santiago Azagra J, et al. Laparoscopic liver resection for malignant liver tumors: preliminary results of a multicenter European study. Ann Surg 2002;236:90-7. [Crossref] [PubMed]
- Belli G, Limongelli P, Fantini C, et al. Laparoscopic and open treatment of hepatocellular carcinoma in patients with cirrhosis. Br J Surg 2009;96:1041-8. [Crossref] [PubMed]
- Truant S, Bouras AF, Hebbar M, et al. Laparoscopic resection vs. open liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: a case-matched study. Surg Endosc 2011;25:3668-77. [Crossref] [PubMed]
- Cheung TT, Dai WC, Tsang SH, et al. Pure Laparoscopic Hepatectomy Versus Open Hepatectomy for Hepatocellular Carcinoma in 110 Patients With Liver Cirrhosis: A Propensity Analysis at a Single Center. Ann Surg 2016;264:612-20. [Crossref] [PubMed]
- Yoon YI, Kim KH, Kang SH, et al. Pure Laparoscopic Versus Open Right Hepatectomy for Hepatocellular Carcinoma in Patients With Cirrhosis: A Propensity Score Matched Analysis. Ann Surg 2017;265:856-63. [Crossref] [PubMed]
- Xu HW, Liu F, Li HY, et al. Outcomes following laparoscopic versus open major hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a propensity score-matched analysis. Surg Endosc 2018;32:712-9. [Crossref] [PubMed]
- Austin PC. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behav Res 2011;46:399-424. [Crossref] [PubMed]
- Kaneko H, Otsuka Y, Tsuchiya M, et al. Application of devices for safe laparoscopic hepatectomy. HPB (Oxford) 2008;10:219-24. [Crossref] [PubMed]
- Dagher I, Caillard C, Proske JM, et al. Laparoscopic right hepatectomy: original technique and results. J Am Coll Surg 2008;206:756-60. [Crossref] [PubMed]
- Santambrogio R, Opocher E, Ceretti AP, et al. Impact of intraoperative ultrasonography in laparoscopic liver surgery. Surg Endosc 2007;21:181-8. [Crossref] [PubMed]
- Lai EC, Tang CN, Ha JP, et al. The evolving influence of laparoscopy and laparoscopic ultrasonography on patients with hepatocellular carcinoma. Am J Surg 2008;196:736-40. [Crossref] [PubMed]
- Araki K, Conrad C, Ogiso S, et al. Intraoperative ultrasonography of laparoscopic hepatectomy: key technique for safe liver transection. J Am Coll Surg 2014;218:e37-41. [Crossref] [PubMed]
- Kosuge T, Makuuchi M, Takayama T, et al. Long-term results after resection of hepatocellular carcinoma: experience of 480 cases. Hepatogastroenterology 1993;40:328-32. [PubMed]
- Hasegawa K, Kokudo N, Imamura H, et al. Prognostic impact of anatomic resection for hepatocellular carcinoma. Ann Surg 2005;242:252-9. [Crossref] [PubMed]
- National Hepatic Surgery Group Society of Surgery CMA. Expert consensus on laparoscopic hepatectomy (2013 version). J Huazhong Univ Sci Technolog Med Sci 2013;33:791-7. [Crossref] [PubMed]
- Coelho FF, Kruger JA, Fonseca GM, et al. Laparoscopic liver resection: Experience based guidelines. World J Gastrointest Surg 2016;8:5-26. [Crossref] [PubMed]
- Sakoda M, Ueno S, Iino S, et al. Anatomical laparoscopic hepatectomy for hepatocellular carcinoma using indocyanine green fluorescence imaging. J Laparoendosc Adv Surg Tech A 2014;24:878-82. [Crossref] [PubMed]
- Ishizawa T, Zuker NB, Kokudo N, et al. Positive and negative staining of hepatic segments by use of fluorescent imaging techniques during laparoscopic hepatectomy. Arch Surg 2012;147:393-4. [Crossref] [PubMed]
- Ishizawa T, Saiura A, Kokudo N. Clinical application of indocyanine green-fluorescence imaging during hepatectomy. Hepatobiliary Surg Nutr 2016;5:322-8. [Crossref] [PubMed]
- Kudo H, Ishizawa T, Tani K, et al. Visualization of subcapsular hepatic malignancy by indocyanine-green fluorescence imaging during laparoscopic hepatectomy. Surg Endosc 2014;28:2504-8. [Crossref] [PubMed]
- Otsuka Y, Kaneko H, Cleary SP, et al. What is the best technique in parenchymal transection in laparoscopic liver resection? Comprehensive review for the clinical question on the 2nd International Consensus Conference on Laparoscopic Liver Resection. J Hepatobiliary Pancreat Sci 2015;22:363-70. [Crossref] [PubMed]
- Buell JF, Gayet B, Han HS, et al. Evaluation of stapler hepatectomy during a laparoscopic liver resection. HPB (Oxford) 2013;15:845-50. [Crossref] [PubMed]
- Rau HG, Duessel AP, Wurzbacher S. The use of water-jet dissection in open and laparoscopic liver resection. HPB (Oxford) 2008;10:275-80. [Crossref] [PubMed]
- Mbah NA, Brown RE, Bower MR, et al. Differences between bipolar compression and ultrasonic devices for parenchymal transection during laparoscopic liver resection. HPB (Oxford) 2012;14:126-31. [Crossref] [PubMed]
- Horgan PG. A novel technique for parenchymal division during hepatectomy. Am J Surg 2001;181:236-7. [Crossref] [PubMed]
- Gertsch P, Pelloni A, Guerra A, et al. Initial experience with the harmonic scalpel in liver surgery. Hepatogastroenterology 2000;47:763-6. [PubMed]
- Harold KL, Pollinger H, Matthews BD, et al. Comparison of ultrasonic energy, bipolar thermal energy, and vascular clips for the hemostasis of small-, medium-, and large-sized arteries. Surg Endosc 2003;17:1228-30. [Crossref] [PubMed]
- Ikegami T, Shimada M, Imura S, et al. Argon gas embolism in the application of laparoscopic microwave coagulation therapy. J Hepatobiliary Pancreat Surg 2009;16:394-8. [Crossref] [PubMed]
- Kono M, Yahagi N, Kitahara M, et al. Cardiac arrest associated with use of an argon beam coagulator during laparoscopic cholecystectomy. Br J Anaesth 2001;87:644-6. [Crossref] [PubMed]
- Huang MT, Lee WJ, Wang W, et al. Hand-assisted laparoscopic hepatectomy for solid tumor in the posterior portion of the right lobe: initial experience. Ann Surg 2003;238:674-9. [Crossref] [PubMed]
- Kurokawa T, Inagaki H, Sakamoto J, et al. Hand-assisted laparoscopic anatomical left lobectomy using hemihepatic vascular control technique. Surg Endosc 2002;16:1637-8. [Crossref] [PubMed]
- Ikeda T, Yonemura Y, Ueda N, et al. Pure laparoscopic right hepatectomy in the semi-prone position using the intrahepatic Glissonian approach and a modified hanging maneuver to minimize intraoperative bleeding. Surg Today 2011;41:1592-8. [Crossref] [PubMed]
- Ikeda T, Mano Y, Morita K, et al. Pure laparoscopic hepatectomy in semiprone position for right hepatic major resection. J Hepatobiliary Pancreat Sci 2013;20:145-50. [Crossref] [PubMed]
- Ikeda T, Toshima T, Harimoto N, et al. Laparoscopic liver resection in the semiprone position for tumors in the anterosuperior and posterior segments, using a novel dual-handling technique and bipolar irrigation system. Surg Endosc 2014;28:2484-92. [Crossref] [PubMed]
- Chen JC, Zhang RX, Chen MS, et al. Left jackknife position: a novel position for laparoscopic hepatectomy. Chin J Cancer 2017;36:31. [Crossref] [PubMed]
- Ban D, Tanabe M, Ito H, et al. A novel difficulty scoring system for laparoscopic liver resection. J Hepatobiliary Pancreat Sci 2014;21:745-53. [Crossref] [PubMed]
- Linden BC, Humar A, Sielaff TD. Laparoscopic stapled left lateral segment liver resection--technique and results. J Gastrointest Surg 2003;7:777-82. [Crossref] [PubMed]
- Chang S, Laurent A, Tayar C, et al. Laparoscopy as a routine approach for left lateral sectionectomy. Br J Surg 2007;94:58-63. [Crossref] [PubMed]
- Belli G, Fantini C, D'Agostino A, et al. Laparoscopic left lateral hepatic lobectomy: a safer and faster technique. J Hepatobiliary Pancreat Surg 2006;13:149-54. [Crossref] [PubMed]
- Wang X, Li J, Wang H, et al. Validation of the laparoscopically stapled approach as a standard technique for left lateral segment liver resection. World J Surg 2013;37:806-11. [Crossref] [PubMed]
- Liu CL, Fan ST, Cheung ST, et al. Anterior approach versus conventional approach right hepatic resection for large hepatocellular carcinoma: a prospective randomized controlled study. Ann Surg 2006;244:194-203. [Crossref] [PubMed]
- Wu TJ, Wang F, Lin YS, et al. Right hepatectomy by the anterior method with liver hanging versus conventional approach for large hepatocellular carcinomas. Br J Surg 2010;97:1070-8. [Crossref] [PubMed]
- Capussotti L, Ferrero A, Russolillo N, et al. Routine anterior approach during right hepatectomy: results of a prospective randomised controlled trial. J Gastrointest Surg 2012;16:1324-32. [Crossref] [PubMed]
- Soubrane O, Schwarz L, Cauchy F, et al. A Conceptual Technique for Laparoscopic Right Hepatectomy Based on Facts and Oncologic Principles: The Caudal Approach. Ann Surg 2015;261:1226-31. [Crossref] [PubMed]
- Cai L, Wei F, Yu Y, et al. Laparoscopic Right Hepatectomy by the Caudal Approach Versus Conventional Approach: A Comparative Study. J Laparoendosc Adv Surg Tech A 2016;26:540-7. [Crossref] [PubMed]
- Takahashi M, Wakabayashi G, Nitta H, et al. Pure laparoscopic right hepatectomy by anterior approach with hanging maneuver for large intrahepatic cholangiocarcinoma. Surg Endosc 2013;27:4732-3. [Crossref] [PubMed]
- Tomishige H, Morise Z, Kawabe N, et al. Caudal approach to pure laparoscopic posterior sectionectomy under the laparoscopy-specific view. World J Gastrointest Surg 2013;5:173-7. [Crossref] [PubMed]
- Nomi T, Fuks D, Agrawal A, et al. Totally laparoscopic right hepatectomy combined with resection of the inferior vena cava by anterior approach. Ann Surg Oncol 2015;22:851. [Crossref] [PubMed]
- Yamashita S, Loyer E, Kang HC, et al. Total Transthoracic Approach Facilitates Laparoscopic Hepatic Resection in Patients with Significant Prior Abdominal Surgery. Ann Surg Oncol 2017;24:1376-7. [Crossref] [PubMed]
- Cai X, Zhao J, Wang Y, et al. A Left-Sided, Purely Laparoscopic Approach for Anatomic Caudate Hepatectomy: A Single-Center Experience. J Laparoendosc Adv Surg Tech A 2016;26:103-8. [Crossref] [PubMed]
- Kwon AH, Matsui Y, Kamiyama Y. Perioperative blood transfusion in hepatocellular carcinomas: influence of immunologic profile and recurrence free survival. Cancer 2001;91:771-8. [Crossref] [PubMed]
- de Boer MT, Molenaar IQ, Porte RJ. Impact of blood loss on outcome after liver resection. Dig Surg 2007;24:259-64. [Crossref] [PubMed]
- Tranchart H, Di Giuro G, Lainas P, et al. Laparoscopic liver resection with selective prior vascular control. Am J Surg 2013;205:8-14. [Crossref] [PubMed]
- Otsuka Y, Katagiri T, Ishii J, et al. Gas embolism in laparoscopic hepatectomy: what is the optimal pneumoperitoneal pressure for laparoscopic major hepatectomy? J Hepatobiliary Pancreat Sci 2013;20:137-40. [Crossref] [PubMed]
- Kobayashi S, Honda G, Kurata M, et al. An Experimental Study on the Relationship Among Airway Pressure, Pneumoperitoneum Pressure, and Central Venous Pressure in Pure Laparoscopic Hepatectomy. Ann Surg 2016;263:1159-63. [Crossref] [PubMed]
- Eiriksson K, Fors D, Rubertsson S, et al. High intra-abdominal pressure during experimental laparoscopic liver resection reduces bleeding but increases the risk of gas embolism. Br J Surg 2011;98:845-52. [Crossref] [PubMed]
- Kawaguchi Y, Fuks D, Kokudo N, et al. Difficulty of Laparoscopic Liver Resection: Proposal for a New Classification. Ann Surg 2018;267:13-7. [Crossref] [PubMed]
- Halls MC, Cherqui D, Taylor MA, et al. Are the current difficulty scores for laparoscopic liver surgery telling the whole story? An international survey and recommendations for the future. HPB (Oxford) 2018;20:231-6. [Crossref] [PubMed]
- Cai X, Li Z, Zhang Y, et al. Laparoscopic liver resection and the learning curve: a 14-year, single-center experience. Surg Endosc 2014;28:1334-41. [Crossref] [PubMed]
- Nomi T, Fuks D, Kawaguchi Y, et al. Learning curve for laparoscopic major hepatectomy. Br J Surg 2015;102:796-804. [Crossref] [PubMed]
- Brown KM, Geller DA. What is the Learning Curve for Laparoscopic Major Hepatectomy? J Gastrointest Surg 2016;20:1065-71. [Crossref] [PubMed]
- Tomassini F, Scuderi V, Colman R, et al. The single surgeon learning curve of laparoscopic liver resection: A continuous evolving process through stepwise difficulties. Medicine (Baltimore) 2016;95. [Crossref] [PubMed]
- van der Poel MJ, Besselink MG, Cipriani F, et al. Outcome and Learning Curve in 159 Consecutive Patients Undergoing Total Laparoscopic Hemihepatectomy. JAMA Surg 2016;151:923-8. [Crossref] [PubMed]
- Hanly EJ, Talamini MA. Robotic abdominal surgery. Am J Surg 2004;188:19S-26S. [Crossref] [PubMed]
- Giulianotti PC, Coratti A, Sbrana F, et al. Robotic liver surgery: results for 70 resections. Surgery 2011;149:29-39. [Crossref] [PubMed]
- Choi GH, Choi SH, Kim SH, et al. Robotic liver resection: technique and results of 30 consecutive procedures. Surg Endosc 2012;26:2247-58. [Crossref] [PubMed]
- Nota CL, Rinkes IHB, Hagendoorn J. Setting up a robotic hepatectomy program: a Western-European experience and perspective. Hepatobiliary Surg Nutr 2017;6:239-45. [Crossref] [PubMed]
- Lai ECH, Tang CN. Training robotic hepatectomy: the Hong Kong experience and perspective. Hepatobiliary Surg Nutr 2017;6:222-9. [Crossref] [PubMed]
- Tsung A, Geller DA, Sukato DC, et al. Robotic versus laparoscopic hepatectomy: a matched comparison. Ann Surg 2014;259:549-55. [Crossref] [PubMed]
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 1997;78:606-17. [Crossref] [PubMed]
- Page AJ, Ejaz A, Spolverato G, et al. Enhanced recovery after surgery protocols for open hepatectomy--physiology, immunomodulation, and implementation. J Gastrointest Surg 2015;19:387-99. [Crossref] [PubMed]
- Liang X, Ying H, Wang H, et al. Enhanced Recovery Program Versus Traditional Care in Laparoscopic Hepatectomy. Medicine (Baltimore) 2016;95. [Crossref] [PubMed]
- Melloul E, Hubner M, Scott M, et al. Guidelines for Perioperative Care for Liver Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J Surg 2016;40:2425-40. [Crossref] [PubMed]
- Gobardhan PD, Subar D, Gayet B. Laparoscopic liver surgery: An overview of the literature and experiences of a single centre. Best Pract Res Clin Gastroenterol 2014;28:111-21. [Crossref] [PubMed]
- Martin RC 2nd, Mbah NA, St Hill R, et al. Laparoscopic versus open hepatic resection for hepatocellular carcinoma: improvement in outcomes and similar cost. World J Surg 2015;39:1519-26. [Crossref] [PubMed]
- Cleary SP, Han HS, Yamamoto M, et al. The comparative costs of laparoscopic and open liver resection: a report for the 2nd International Consensus Conference on Laparoscopic Liver Resection. Surg Endosc 2016;30:4691-6. [Crossref] [PubMed]
- Kawaguchi Y, Otsuka Y, Kaneko H, et al. Comparisons of financial and short-term outcomes between laparoscopic and open hepatectomy: benefits for patients and hospitals. Surg Today 2016;46:535-42. [Crossref] [PubMed]


