Should we expand liver transplant criteria to cirrhotic patients with intrahepatic cholangiocarcinoma?
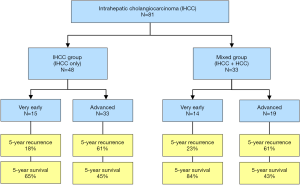
Liver transplantation (LT) for “very early” intrahepatic cholangiocarcinoma (IHCC) in patients with end-stage liver disease (ESLD) has been advocated by the IHCC International Consortium based on a recently published multicenter study (1). The authors of this study retrospectively collected data from 81 liver transplant recipients who had confirmed histology of IHCC on explant pathology either diagnosed as preoperatively expected (n=65) or incidentally found (n=16). Out of the 81 patients, 48 had IHCC while 38 had mixed biphenotypic features of IHCC and hepatocellular carcinoma (HCC). Tumors were classified into two categories: very early (single tumor <2 cm) and advanced (single tumor >2 cm or multiple tumors) tumors. The central finding of this study was the favorable post-transplant outcome of patients with very early IHCC that compares to outcome accepted for HCC. The 5-year recurrence and survival rates of the very early group were 18% and 65% for IHCC and 23% and 84% for mixed IHCC/HCC while both outcome rates were considerably worse for the advanced group (Figure 1).
While LT criteria have been established for hilar cholangiocarcinoma, accepted guidelines for LT in patients with IHCC are lacking. For unresectable perihilar cholangiocarcinoma, T1-3 tumors with a tumor mass ≤3 cm and no evidence of lymph node metastases (N0) are widely accepted criteria to be considered for LT (2). Of note, the vast majority of patients with hilar cholangiocarcinoma has no underlying chronic liver disease except those suffering from primary sclerosing cholangitis (PSC). However, the study of the IHCC International Consortium addresses IHCC in patients with ESLD. While liver resection remains the treatment of choice for IHCC in non-cirrhotic patients (3), the International Consortium group advocates LT in patients with IHCC when patients suffer from ESLD and when the tumor disease is restricted to a single lesion with a size of less than 2 cm (1). The preoperative establishment of the diagnosis “very early” IHCC might be challenging due to the small tumor size. This diagnostic problem is also mirrored by the findings of the International Consortium study where IHCC was incidentally found in the explant specimen of a significant proportion of patients (20%) at time of LT.
The International Consortium study identified microvascular invasion and poor differentiation as independent risk factors for post-transplant tumor recurrence, but surprisingly, the category “advanced” tumor did not come out as independent predictor of recurrent disease in this study (1). This might be attributed to the relatively small study population but may also imply that tumor biology appears more important for post-transplant prognosis than tumor category alone defined by number and size of tumor lesions. Other studies have shown that biological characteristics of IHCC such as perineural invasion (4,5), tumor differentiation (6), and lymphovascular invasion (4) have prognostic impact after LT (Table 1). A recently published study from the University of California Los Angeles proposed a predictive risk index for tumor recurrence after LT for locally advanced intrahepatic and hilar cholangiocarcinoma (4). In this study, tumor biology criteria such as multifocality, perineural invasion, infiltrative growth as well as lymphovascular invasion were important risk factors for recurrent disease after LT. Based on a predictive index of these criteria, the authors of the same study defined a low risk group, which had a favorable 5-year recurrence-free survival rate of 78% after LT (Table 1). The low risk group was predominantly composed of single IHCC (82%) with a mean tumor diameter of 6.2 cm. Interestingly, the mean tumor diameter of 6.2 cm is far above the proposed 2-cm threshold of the International Consortium study and challenges the importance of tumor biology over tumor size in single IHCC. Furthermore, the authors discuss the scenario of tumor growth of very early IHCC while awaiting LT (1). They speculate that a growth to 3 cm should not be considered as drop-out criterion preventing patients from LT. This statement might be even more valid when IHCC lesions have favorable tumor biology on histology (4). Therefore, future prospective studies with a larger study population should focus on refinement of selection criteria for LT in patients with IHCC in terms of tumor biology and intrahepatic tumor burden (number and size).

Full table
Regardless of the underlying liver disease, cirrhotic liver parenchyma is a well-known risk factor for the development of HCC. This is less the case for IHCC except for patients suffering from PSC. Therefore, the question arises whether cirrhotic patients with small IHCC (very early) and well-compensated liver function [laboratory model of end-stage liver disease (MELD) >15] who do not have underlying PSC should undergo LT or whether these patients would better benefit from resection or ablative therapy. Another important objective of future studies might be to investigate if successful downstaging of single advanced IHCC lesion to very early criteria is accepted to proceed with LT or remains associated with the unfavorable prognosis observed for the advanced IHCC group.
An important issue of LT for IHCC is related to the regional lymph node status. It is well known that regional lymph node metastases are an important predictor for reduced patient survival after liver resection for IHCC (3,7). Furthermore, the absence of regional lymph node metastases is a mandatory selection criterion established for LT in patients with hilar cholangiocarcinoma, which requires explorative staging lymphadenectomy of the hepatoduodenal ligament before LT (2). On the other hand, the likelihood of regional lymph node metastases in very early IHCC is uncertain and has not been answered by the International Consortium study. As the authors stated in their publication (1), information on regional lymph nodes were scare in their study. Similar to LT for HCC within accepted criteria [Milan, University of California San Francisco (UCSF)], regional lymph node metastases might not play an important role in very early IHCC. However, future prospective studies should also integrate staging lymphadenectomy of the hepatoduodenal ligament at time of LT to answer whether node positivity appears either an important or an insignificant issue in very early IHCC. Staging lymphadenectomies before LT as performed in non-cirrhotic patients with hilar cholangiocarcinoma should not be advised in patients with ESLD due to the potential risk of hepatic decompensation.
Although there is well-documented evidence of the diagnostic importance of positron emission tomography/computed tomography (PET/CT) in cholangiocarcinoma, the authors of the International Consortium study did not make any recommendation in terms of imaging for preoperative work-up. Especially for IHCC, PET/CT has a high diagnostic accuracy for both primary tumor and distant metastases (8-10). Therefore, this imaging modality, where available, should be a mandatory element of the diagnostic work-up before LT when IHCC is either supposed or histologically confirmed.
In conclusion, the authors of the IHCC International Consortium advocate LT in cirrhotic patients with very early IHCC. LT in this highly selected population appears justified due to the associated favorable post-transplant prognosis that compares to outcome accepted for HCC. This observation is based on the largest multicenter report of LT for IHCC. However, many important questions remain unanswered and should be goals of future prospective studies.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Sapisochin G, Facciuto M, Rubbia-Brandt L, et al. Liver transplantation for "very early" intrahepatic cholangiocarcinoma: International retrospective study supporting a prospective assessment. Hepatology 2016;64:1178-88. [Crossref] [PubMed]
- Mansour JC, Aloia TA, Crane CH, et al. Hilar cholangiocarcinoma: expert consensus statement. HPB (Oxford) 2015;17:691-9. [Crossref] [PubMed]
- Weber SM, Ribero D, O'Reilly EM, et al. Intrahepatic cholangiocarcinoma: expert consensus statement. HPB (Oxford) 2015;17:669-80. [Crossref] [PubMed]
- Hong JC, Petrowsky H, Kaldas FM, et al. Predictive index for tumor recurrence after liver transplantation for locally advanced intrahepatic and hilar cholangiocarcinoma. J Am Coll Surg 2011;212:514-20; discussion 520-1. [Crossref] [PubMed]
- Robles R, Figueras J, Turrion VS, et al. Spanish experience in liver transplantation for hilar and peripheral cholangiocarcinoma. Ann Surg 2004;239:265-71. [Crossref] [PubMed]
- Takahashi K, Obeid J, Burmeister CS, et al. Intrahepatic Cholangiocarcinoma in the Liver Explant After Liver Transplantation: Histological Differentiation and Prognosis. Ann Transplant 2016;21:208-15. [Crossref] [PubMed]
- Raoof M, Dumitra S, Ituarte PH, et al. Development and Validation of a Prognostic Score for Intrahepatic Cholangiocarcinoma. JAMA Surg 2017;152:e170117. [Crossref] [PubMed]
- Jiang L, Tan H, Panje CM, et al. Role of 18F-FDG PET/CT Imaging in Intrahepatic Cholangiocarcinoma. Clin Nucl Med 2016;41:1-7. [Crossref] [PubMed]
- Lee Y, Yoo IR, Boo SH, et al. The Role of F-18 FDG PET/CT in Intrahepatic Cholangiocarcinoma. Nucl Med Mol Imaging 2017;51:69-78. [Crossref] [PubMed]
- Petrowsky H, Wildbrett P, Husarik DB, et al. Impact of integrated positron emission tomography and computed tomography on staging and management of gallbladder cancer and cholangiocarcinoma. J Hepatol 2006;45:43-50. [Crossref] [PubMed]


