Left hepatectomy with concomitant cavo-atrial and biliary tumor thrombectomy for invasive hepatocellular carcinoma: a video report
Introduction
Representing the prevalent primary hepatic malignancy, hepatocellular carcinoma (HCC) is concurrently the sixth most common cancer worldwide and the third dominant cause of mortality due to cancer (1,2).
The preponderance of such neoplasms is secondary to cirrhosis, primarily induced by viral hepatitis, alcohol abuse or exposure to other hepatotoxins. Over the last decades, however, metabolic disorders such as obesity and insulin resistance, have established as key players in the chronic damage of liver parenchyma, eventually contributing to the development of the large spectrum of chronic hepatopathies known as non-alcoholic fatty liver disease (NAFLD) (3).
HCC displays a high affinity towards the vascular system as demonstrated by the frequently reported invasion of the portal vein. On the other hand, neoplastic extension to hepatic veins or to the biliary tract have been seldom described (1,4).
Herein, we present the singular case of a 76-year-old man affected by cryptogenic cirrhosis (Child-Pugh score B7 and model for end stage liver disease 12), presumably owing to NAFLD, with a left lobe voluminous HCC displaying a tumor extension through the left hepatic vein and inferior vena cava (IVC) reaching the right atrium, concurrently to a left hepatic duct neoplastic thrombosis. This case represents a rare occurrence and is the first reported case of HCC with concomitant hepatic vein-cavo-atrial and biliary tumor invasion.
The patient denied consumption of alcoholic beverages and serology was negative for viral hepatitis panel. Comorbid conditions comprised hypertension, grade 1 obesity (BMI 33.8 kg/m2) and a recent onset of paroxysmal atrial fibrillation. A presumed diagnosis of NAFLD-related cirrhosis was made on the basis of clinical, laboratory and radiological features.
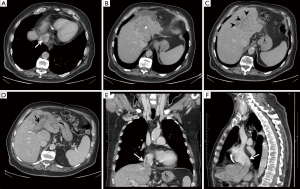
Preoperative computed tomography (CT) findings are illustrated in Figure 1.
After a multidisciplinary evaluation and in consideration of the extension of the tumor, additionally to previous laparotomic surgeries, decision was made to proceed to a left hepatectomy with cavo-atrial and biliary thrombectomy through an open abdominal approach.
Surgical technique
The patient was placed on the operative table in supine position and access to the abdominal cavity was gained through a Makuuchi incision. The liver parenchyma was examined by intraoperative ultrasonography to confirm vasculobiliary anatomy, extension of the HCC and for demarcation of exact parenchymal transection line. The liver was freed from its ligamentous attachments and the IVC was exposed and encircled in its infrahepatic portion. Pringle’s maneuver was performed for transient inflow occlusion, hepatic pedicle was exposed and hilum elements were separately isolated. Ligation and division of the left hepatic artery and left portal vein was achieved. Transection of the liver parenchyma was thus commenced using an ultrasonic sealing device. During transection of hepatic parenchyma, a markedly dilated left hepatic duct was encountered and intraoperative ultrasound showed the presence of a solid mass within its lumen. The duct was sectioned and a biliary thrombus was noted and removed (Figure 2A,B). Following completion of dissection up to the posterior hepatic margin, the common trunk of left and middle hepatic veins was isolated. An opening was then performed on the central tendon of the diaphragm, the supra- and infradiaphragmatic IVC was exposed and encircled for control and in order to safely excise the intracavo-atrial tumor. Hepatic pedicle and IVC clamping was transiently required during cavo-atrial thrombectomy. Finally, a left hepatectomy with ‘en bloc’ cavo-atrial thrombectomy (Figure 2C,D) was successfully performed and the left and middle common hepatic trunk stump was sutured with non-absorbable material. Operative time was 316 min and total blood loss estimation was 200 mL. Postoperative course was uneventful and the patient was discharged on postoperative day 7.
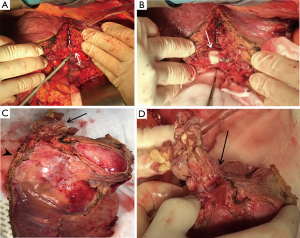
Histopathological examination confirmed the diagnosis of a poorly differentiated HCC (WHO G3; Modified Edmondson-Steiner grade III), with direct infiltration of the left and middle hepatic vein and left hepatic duct amidst a micro-macronodular cirrhotic liver parenchyma.
At 3 months follow-up the patient did not show evidence of disease recurrence.
An additional movie file shows the surgical procedure in detail (Figure 3).

Discussion
HCC accounts for 90% of primary hepatic malignancies. Its 5-year survival rate has been estimated to be as low as 5% in the subpopulation of non-transplantable patients (2).
HCC is endowed with a highly aggressive potential, possibly giving rise to tumor growth within blood vessels and resulting in neoplastic thrombosis of major vasculature, due to its remarkable vascular affinity. Widely reported in literature is the involvement of the portal system, variably described as an autoptic finding in 26–80% of HCCs, carrying a well-defined negative prognostic value (1,6). In contrast, IVC or right atrium involvement via the hepatic veins is a less frequent occurrence, displaying an incidence of 0.53% and noted in merely 6% of post-mortem autopsies (2).
At present, no definitive global consensus or agreement has been reached regarding the management of HCC with IVC or cardiac tumor thrombosis. This is possibly due to the fact that patients with vascular neoplastic involvement, hence an advanced disease stage, do not meet traditional criteria for surgery because of reportedly poor postoperative outcomes. A surgical approach, associating liver resection with thrombectomy is apparently the sole possibility, among the available therapeutic armamentarium, for a radical tumor removal (6). Patients presenting with extensive tumor thrombus extension to the right atrium or further, may require a multidisciplinary approach inclusive of extracorporeal circulation. Surgery represents a potential treatment in cases where the primary tumor has characteristics of resectability and the estimated future liver remnant is sufficient to prevent postoperative hepatic failure. Nonetheless, effective oncological advantages in terms of overall survival after surgical treatment are currently uncertain. Available evidence predominantly includes case series and reports which do not allow to draw unbiased results and make definitive conclusions regarding survival advantages in this subgroup of patients (1,6).
In conclusion, the prevalence of HCC is likely to rise due to the broad increase of worldwide obesity, with particular distribution within Western countries. Therapeutic and life-lengthening management options are various, although not all are endowed with curative intent. Nevertheless, treatment of HCC with vascular or bile duct extension poses further challenges. Amongst therapeutic approaches, hepatic resection associated with vascular and biliary thrombectomy displays a potentially favorable outcome in terms of overall survival and represents a viable option in selected patients. Nonetheless, randomized controlled trials are essential in order to validate treatment modality choice.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- An J, Lee KS, Kim KM, et al. Clinical features and outcomes of patients with hepatocellular carcinoma complicated with bile duct invasion. Clin Mol Hepatol 2017;23:160-9. [Crossref] [PubMed]
- Oncale M, Lewis B. Hepatocellular carcinoma with extension to the heart via the inferior vena cava. Proc (Bayl Univ Med Cent) 2015;28:229-30. [Crossref] [PubMed]
- Clark JM, Diehl AM. Nonalcoholic fatty liver disease: an underrecognized cause of cryptogenic cirrhosis. JAMA 2003;289:3000-4. [Crossref] [PubMed]
- Sung AD, Cheng S, Moslehi J, et al. Hepatocellular carcinoma with intracavitary cardiac involvement: a case report and review of the literature. Am J Cardiol 2008;102:643-5. [Crossref] [PubMed]
- Castagneto Gissey L, Musleh L, Mariano G, et al. Video case illustrating in detail the biliary and intracaval-intracardiac tumor thrombus removal. Asvide 2018;5:387. Available online: http://www.asvide.com/article/view/24122
- Wang Y, Yuan L, Ge RL, et al. Survival benefit of surgical treatment for hepatocellular carcinoma with inferior vena cava/right atrium tumor thrombus: results of a retrospective cohort study. Ann Surg Oncol 2013;20:914-22. [Crossref] [PubMed]


