Monosegment ALPPS hepatectomy preserving segment 4 for colorectal liver metastases: literature review and our experience
Introduction
Monosegment Associating Liver Partition and Portal Vein ligation for Staged hepatectomy (ALPPS) was defined by Schadde et al. as a liver resection leaving a remnant constituted of one single segment ± segment 1 (S1) (1). This variation of the ALPPS technique represents a substantial change to the traditional paradigm of liver resectability, which is defined as the removal of tumour with negative margins, preserving ≥2 contiguous liver segments along with their inflow, outflow and biliary drainage. Various reports and reviews have been published, describing advantages and limitations of ALPPS (1-3). ALPPS induces a rapid hypertrophy of the liver remnant compared to portal vein embolization or ligation with a rate of completion of second stage between 95% and 100%. However, concerns are mainly due to the high morbidity (up to 44% of Clavien-Dindo grade III or more) and mortality rates up to 29%, as well as the possible relationship between a rapid hypertrophy and tumour progression (3). Therefore, ALPPS is still a debated topic. Monosegment ALPPS hepatectomy overcomes left and right trisectionectomy, which are the most extensive liver resections according to the terminology introduced by the IHPBA (4), with the intent of offering an oncological resection and a lower incidence of post-hepatectomy liver failure (PHLF). Prior to the introduction of ALPPS, the treatment of bilobar borderline resectable liver metastases with single segment remnants could only be achieved by the means of two-stage hepatectomies (TSH), but often requiring very long intervals to achieve a sufficient FLR. Alternatively, the option of ultrasound-guided multiple wedge resections aimed to maximize parenchymal-sparing and to allow curative resection in one stage (5,6).
However, the ALPPS technique has not yet been standardized. Different types of monosegment ALPPS hepatectomy have been described by Schadde et al., who proposed a nomenclature based on the segment of the liver remnant rather than the segments of resected liver (2). In this report, we present our preliminary experience on segment 4+1 monosegment ALPPS hepatectomy and a review of the literature of published similar cases.
Methods
Literature search
PubMed database was searched from inception to 23/10/2016. The following search terms were used: Text words [monosegment*] AND [ALPPS*] OR [Associating Liver Partition and Portal Vein ligation for Staged hepatectomy*]. Three results were yielded in total from the initial search.
Definitions
Segments were defined according to the classic Couinaud’s anatomical division of the liver (7). Monosegment resection was defined as a liver resection leaving a remnant constituted of 1 single segment ±S1 (2). The cut-off for the minimal safe size of the liver remnant after single stage hepatectomy was set as >30% of the TLV for patients with chemotherapy-related liver injury (8). Post-hepatectomy liver failure (PHLF) was defined according to the International Study Group of Liver Surgery (ISGLS) classification (increased INR or need of clotting factors to maintain normal INR and hyperbilirubinemia on or after postoperative day 5) (9). Postoperative complications were graded according to the Clavien-Dindo classification (10).
Patients
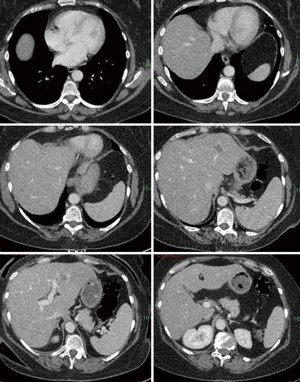
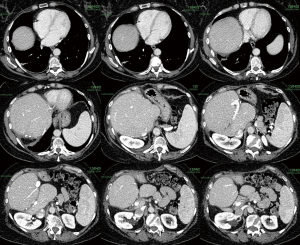
Two patients underwent segment 4+1 ALPPS hepatectomy at Aberdeen Royal Infirmary (UK). The first patient was a 61-year-old female with no comorbidities. She presented with adenocarcinoma of the right colon with synchronous bilobar liver metastases. The preoperative CT and MRI liver showed 7 lesions in segments 5, 7 and 8 and in the left lobe, where the largest, measuring 3.4 cm, was at the passage between S2 and S3. She underwent right hemicolectomy, and the primary was staged as Duke’s D pT3N1. After chemotherapy with four cycles of Capecitabine and Oxaliplatin (XELOX), a partial response was observed. Technically, the right hemiliver and the left lateral sector could not be preserved due to the involvement of the right hepatic vein and the large lesion in S2−3. The preoperative FLR volume for segments 4+1 was 199 cm3, 13% of total liver volume (TLV), which was deemed too small for a single stage procedure (Figure 1).
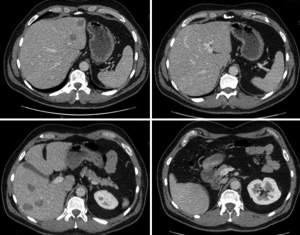
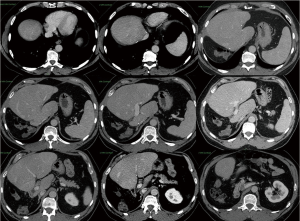
The second patient was a 61-years-old male presenting with mid rectum adenocarcinoma treated with neoadjuvant pelvic radiotherapy, chemotherapy with XELOX and anterior resection with loop ileostomy (stage pT2N1 Duke’s C). He received postoperative Capecitabine alone and unfortunately developed serious drug-induced neuropathy and pulmonary embolism (PE), which required therapeutic dose anticoagulation and contraindicated any further chemotherapy. Six months after resection of the primary tumor, he developed a total of 7 bilobar liver metastases, located in segments 2, 3, 5, 6 and 8. The maximum diameter of the largest lesion was 3cm, deep in S6 close to the sectorial division of the right portal vein. Only segment 7, 4 and 1 were clear from lesions. He could not receive further chemotherapy, and he was offered ALPPS as a rescue approach. The preoperative FLR volume for segments 4 and 1 was 255 cm3, 14% of TLV, which was deemed insufficient to undergo one-stage hepatectomy (Figure 2). For both patients, alternative treatment strategies were evaluated in our institutional Hepatobiliary and Pancreatic Multidisciplinary Meeting (HPB-MDT). Both patients were informed about surgical and nonsurgical options and gave informed consent to undergo two-stage hepatectomy with ALPPS technique.
Technique
First stage consisted in a left lateral sectionectomy with intra-glissonian dissection of the vascular elements assuring the preservation of the artery for segment 4 and its glissonian pedicle. The right portal vein was then ligated and the Cantlie line used as the mark for the right-sided transection. Parenchymal transection was performed using Thunderbeat® (Olimpus) device, whereas clips and ligatures were used for vascular and bile ducts larger than 2 mm in diameter. No vascular occlusion was performed. A fibrin sealant patch (TachoSil®) was used to cover the transection area.
Second stage consisted of the division of right hepatic vein (RHV) and artery (RHA) and right glissonian pedicle with Vascular Endo GIATM with removal of the right hemiliver.
Imaging
Patients were investigated with a preoperative MRI, a triple phase CT and liver volumetry preoperatively, after first stage and postoperatively as part of the follow up. Liver volumes were calculated using FIJI® CT volumetry software on the portal phase.
Results
Institutional experience
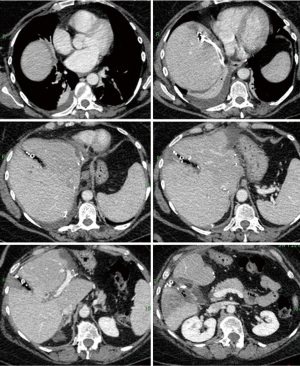
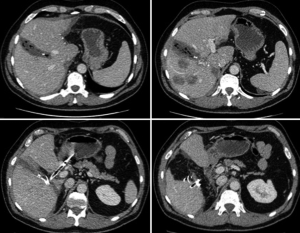
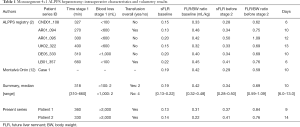
The preoperative volumetry showed total liver volumes of 1,840 and 1,634 cm3. The volume of the FLR, constituted of segment 4+1, was 255 cm3 (patient 1) and 199 cm3 (patient 2). After first stage, a significant FLR growth was observed in both patients: the CT scan prior to stage 2 showed an increase by 165% (255 to 677 cm3) and 241% (199 to 679 cm3), respectively. Second stage was performed after 9 and 14 days, respectively (Figures 3,4). First-stage lasted 6 and 5.5 hours in patient 1 and 2, and both had blood losses above 2,000 mL, requiring intraoperative blood transfusions. Between stages, both patients developed grade A PHLF, not requiring any change in their management. After second-stage both developed mild ascites, which recovered with conservative treatment. Both patients developed a subphrenic intraabdominal collection after second stage, and they required percutaneous drainage. These complications were scored grade IIIa Clavien-Dindo. No 90-day mortality was observed. Histopathology showed a complete resection (R0) in both cases. Both patients are still alive after 20 and 27 months, respectively, with no evidence of recurrent disease (Figures 5,6).
Review of the literature
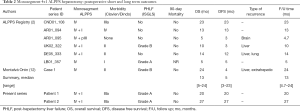
The literature search provided three results, including an original article and two case reports. Schadde et al. (2) analyzed retrospectively the ALPPS Registry for all monosegment ALPPS. In this series 12 patients underwent monosegment ALPPS and 6 of them were segment 4±1 ALPPS. One of the two case reports was already been included within the series published by Schadde (11). Montalvá Orón et al. reported the case of a 65-year-old patient with CRLM who underwent segment 4+1 ALPPS (12). Table 1 shows intraoperative details and volumetrics for the seven cases from the literature and our two patients for comparison. Our cases had a lower baseline FLR and a higher FLR before stage 2 compared to the median values from the literature. Likewise, there was an increase in FLR/BW ratio from 0.31 to 0.84 in patient 1 and from 0.22 to 0.76 in patient 2, compared to median values of 0.42 and 0.69 respectively at baseline and prior to stage 2 in the data from the literature. Median overall survival (OS) for the 7 cases reported in the literature was 13 months (range, 5–24 months). Median disease free survival (DFS) was 5 months (range, 3–23 months), as shown in Table 2: three out of 7 patients did not present recurrence after 5, 13 and 23 months of follow up. Three patients recurred within 6 months: two to the liver and extrahepatic recurrence and one patient with brain metastases. Another patient presented recurrent disease only after 12 months of follow up.
Full table
Full table
Discussion
The two patients presented above had extensive multifocal bilobar CRLM, presenting with more than 6 lesions distributed in less than 6 segments, but with the possibility of a complete oncological resection with negative margins (R0). Therefore, they were considered technically resectable with a two stage hepatectomy (left lobe wedge resections and right hepatectomy) or a monosegment ALPPS. A two stage hepatectomy was technically feasible but, similarly to the cases reported in the literature, the right hemiliver and the LLS could not be retained as part of the FLR and wedge resections of the LLS were considered oncologically inadequate. Monosegment ALPPS was chosen as a salvage procedure with the aim to avoid the risk of drop-out due to inadequate hypertrophy or progression between stages.
Monosegment 4+1 ALPPS hepatectomy in the two cases reported allowed obtaining an oncological clearance of the liver with acceptable costs in term of morbidity and good long-term outcomes.
In the literature, the technique of monosegment ALPPS resection was initially presented as a case report by De Santibanes et al., and then described by Schadde et al. in a subanalysis of the ALPPS Registry (2,11). From a technical point of view, we used the same technique, avoiding the utilization of a plastic sheath on the transection plane and using TachoSil® instead. This decision was made to prevent the need for a surgical removal in case of impossibility to proceed to second stage.
In ALPPS the observed median kinetic growth is 0.02 sFLR per day (interquartile range, 0.01–0.03), which means that a patient with an initial FLR of 15% could achieve the volume cut-off of 30% within 15 days after stage 1 (13). It would require about six weeks to get the same results after TSH, when the liver volume only increases by 2% per week. Furthermore, the risk of cancellation of second stage because of insufficient growth of FLR or further intra or extra-hepatic spread of the disease in the waiting time is more than 35% with TSH (2,4). Overall, ALPPS induces a growth of FLR of approximately 80% in 7 days (range, 6–13 days) with only 3% of patients not undergoing the second stage (13). In our experience of monosegment 4±1 ALPPS and in the literature, second stage was performed in all cases, achieving a complete oncological resection.
The present manuscript and the review of the literature report encouraging oncological outcomes for monosegmental 4±1 ALPPS. Considering all nine cases, overall median disease free survival was 8.5 months (3–27 months) and 5 out of 9 patients did not present any recurrence during their follow up. However, some patients recurred within 6 months with local or extrahepatic disease. Early postoperative recurrence or disease progression in less than 6 months might reflect both a failure of the treatment and a very aggressive biology of the tumor.
Olthof et al. showed that ALPPS had the same outcomes as palliative chemotherapy in patients with at least 2 of the following criteria: ≥6 metastases, ≥2 future liver remnant metastases, ≥6 involved segments excluding segment 1 (14). These results might help in the selection of patients to exclude from ALPPS because of advanced disease, although our two patients met only one of the criteria. However, the number of cases is too small to draw any definitive conclusions regarding the oncological outcomes of monosegment ALPPS.
Monosegment ALPPS might prove of benefit in the future for patients with lesions in proximity of main vascular structures for which a progression in size between stages would compromise the resection. In this group of patients, it seems reasonable to offer an operation with the highest rate of hypertrophy and a completion of stages in the shortest interval possible. Therefore, in our opinion monosegmental ALPPS may represent an appropriate option in a selected group of patients.
To date, monosegment ALPPS is not a standard technique in the treatment of bilateral CRLM. Pringle manoeuvre, diseased liver parenchyma (steatosis, fibrosis, chemotherapy-related changes) and age greater than 60 years may negatively affect kinetic growth (13) and consequently, postoperative outcomes. Bell and colleagues recently investigated the impact of advancing age on short and long term outcomes after major surgery for colorectal liver metastases. Choosing a cut off of 75 years of age, they showed that the elderly group had greater morbidity (P=0.048), whereas marginally statistically significant. The 90-day mortality compared to the <75 group when performing a major hepatectomy of three or more segments was similar in both groups (15). Considering the increase in life expectancy in the western population and the good functional status of many people over 60 there is an open discussion about the differences between chronological and biological age (16). Our two patients were aged 61 at the time of surgery, which is one of the risk factors identified in the ALPPS Registry for poor postoperative outcomes, but they both had a good performance status, without major cardiovascular or respiratory comorbidities to contraindicate major surgery.
Several factors such as experience of each centre, age and patients’ comorbidities should be considered before choosing between TSH and Monosegment ALPPS (17,18). A recent retrospective case-match analysis of ALPPS and TSH for CRLM showed that there was no difference in feasibility and completion of treatment. ALPPS patients had a shorter interval between stages, but at the expense of increased overall and major complications. Interestingly, patients undergoing TSH who matched out from the analysis had a higher ASA score, more lesions and received less chemotherapy than the subgroup used for the matched analysis (19). Those results may confirm that, to date, ALPPS is performed in patients with better performance status and fewer comorbidities and who required more chemotherapy to achieve resectability. Therefore, even though good results have been achieved so far, prospective and randomized studies are needed to clarify the criteria to select the best candidate for ALPPS.
Conclusions
Our results, along with the review of the literature, suggest that the monosegment 4±1 ALPPS procedure is feasible and effective in selected patients. Therefore, it could be a rescue option decreasing the risk of drop-out of the two stage hepatectomy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
References
- Schadde E, Schnitzbauer AA, Tschuor C, et al. Systematic review and meta-analysis of feasibility, safety, and efficacy of a novel procedure: associating liver partition and portal vein ligation for staged hepatectomy. Ann Surg Oncol 2015;22:3109-20. [Crossref] [PubMed]
- Schadde E, Malago M, Hernandez-Alejandro R, et al. Monosegment ALPPS hepatectomy: extending resectability by rapid hypertrophy. Surgery 2015;157:676-89. [Crossref] [PubMed]
- Lau WY, Lai EC, Lau SH. Associating liver partition and portal vein ligation for staged hepatectomy: the current role and development. Hepatobiliary Pancreat Dis Int 2017;16:17-26. [Crossref] [PubMed]
- Terminology Committee of the IHPBA. Terminology of liver anatomy and resections. HPB Surg 2000;2:333-9.
- Adam R, Laurent A, Azoulay D, et al. Two-stage hepatectomy: A planned strategy to treat irresectable liver tumors. Ann Surg 2000;232:777-85. [Crossref] [PubMed]
- Torzilli G, Procopio F, Botea F, et al. One-stage ultrasonographically guided hepatectomy for multiple bilobar colorectal metastases: a feasible and effective alternative to the 2-stage approach. Surgery 2009;146:60-71. [Crossref] [PubMed]
- Bismuth H. Surgical anatomy and anatomical surgery of the liver. World J Surg 1982;6:3-9. [Crossref] [PubMed]
- Nordlinger B, Van Cutsem E, Gruenberger T, et al. Combination of surgery and chemotherapy and the role of targeted agents in the treatment of patients with colorectal liver metastases: recommendations from an expert panel. Ann Oncol 2009;20:985-92. [Crossref] [PubMed]
- Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 2011;149:713-24. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- de Santibañes M, Alvarez FA, Santos FR, et al. The associating liver partition and portal vein ligation for staged hepatectomy approach using only segments I and IV as future liver remnant. J Am Coll Surg 2014;219:e5-9. [Crossref] [PubMed]
- Montalvá Orón EM, Maupoey Ibáñez J, Bañuelos Carrillo R, et al. Monosegment ALPPS: A new variant of the techniques for rapid hepatic regeneration. Critical review of the initial results of our series. Cir Esp 2015;93:436-43. [PubMed]
- Schadde E, Ardiles V, Robles-Campos R, et al. Early survival and safety of ALPPS: first report of the International ALPPS Registry. Ann Surg 2014;260:829-36; discussion 836-8. [Crossref] [PubMed]
- Olthof PB, Huiskens J, Wicherts DA, et al. Survival after associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) for advanced colorectal liver metastases: A case-matched comparison with palliative systemic therapy. Surgery 2017;161:909-19. [Crossref] [PubMed]
- Bell R, Pandanaboyana S, Nisar S, et al. The Impact of Advancing Age on Recurrence and Survival Following Major Hepatectomy for Colorectal Liver Metastases. J Gastrointest Surg 2017;21:266-74. [Crossref] [PubMed]
- Turner NJ, Haward RA, Mulley GP, et al. Cancer in old age--is it inadequately investigated and treated? BMJ 1999;319:309-12. [Crossref] [PubMed]
- Al-Refaie WB, Parsons HM, Henderson WG, et al. Major cancer surgery in the elderly: results from the American College of Surgeons National Surgical Quality Improvement Program. Ann Surg 2010;251:311-8. [Crossref] [PubMed]
- Farges O, Goutte N, Bendersky N, et al. Incidence and risks of liver resection: an all-inclusive French nationwide study. Ann Surg 2012;256:697-704; discussion 704-5. [Crossref] [PubMed]
- Ratti F, Schadde E, Masetti M, et al. Strategies to Increase the Resectability of Patients with Colorectal Liver Metastases: A Multi-center Case-Match Analysis of ALPPS and Conventional Two-Stage Hepatectomy. Ann Surg Oncol 2015;22:1933-42. [Crossref] [PubMed]