Use of robotics in liver donor right hepatectomy
Since the introduction of liver transplantation in 1963, the procedure has been considered the most effective solution for liver failure and other difficult-to-treat liver parenchymal diseases (1,2). Nowadays, the living-related donor right hepatectomy has provided a common graft source in adults given the unstable supply of deceased donor organs (3-5). However, with loss of approximately two thirds of liver for functional liver for the donor, healthy individuals who are volunteering to be donors risk life and recovery (6).
Laparoscopy has been one of the most important surgical innovations, and has been well accepted to produce less postoperative pain, reduced morbidity, and faster recovery. After Caroli et al. introduced laparoscopy to liver surgery in 1955, the adoption of minimally invasive approach to hepatectomy has increased with improvements of the video image system and innovations in surgical instrumentation. However, the progress of the minimally invasive major liver resection has been slow, with the percentage of major resection remaining at 16% to 22% in last five years in most major series of MIS liver resection (7,8).
Improving donor outcome through minimally invasive approach
The transplant surgeon is expected to produce ever decreasing the complication rates and offer better recovery for the donors in order to make donation attractive and to maintain an adequate pool of donor candidates. However, the shortage of donors has been pushing the transplantation community to consider extended selection criteria for the donor candidates. Transplantation surgeons are increasingly willing to accept donors with more complicated anatomy variations and with overweight stature. With expanded donor selection criteria as the solution to the donor shortage, it is likely to increase complication rates of living-related liver donation (9). Moreover, traditional laparotomy results in post-operative suffering, with at least 30% to 50% of the complications in donor hepatectomy appeared to be related to abdominal wall trauma, including hernia, bowel obstruction, and chronic abdominal discomfort (10). One of the major advantages of minimally invasive surgery (MIS) is elimination of the long incision scar, and thus improvement of post-operative recovery. Transplant surgeons have been exploring the possibility that MIS donor harvest can improve outcome for the liver donor. To bridge the gap between open and pure MIS donor procurement, hand-assisted laparoscopic surgery was introduced since the early 1990s. Video-assisted surgery decreased the need for a large wound size, and thus facilitated the procedure. Additionally, experience with pure laparoscopic liver resection has been encouraging a similar approach for donor procurement. Finally in 2002, Cherqui and Soubrane presented the first two cases of laparoscopic living donor hepatectomy for liver transplantation in children (11). The result for these two cases of left liver procurement was inspiring for the initiation of pure laparoscopic donor procedure and symptomless perioperative course of the donors.
From left-sided to right-sided donor hepatectomy
Laparoscopic left lateral liver resection was suggested as routine approach regarding the consensus on laparoscopic liver surgery in 2008 (12). Development of a purely laparoscopic left liver donor procedure follows logically as experience with laparoscopic hepatectomy has increased. Soubrane et al. documented the first comparison between laparoscopic and open left lateral donor hepatectomy with 16 laparoscopic candidates in 2006 (13), in which the procedure was suggested as a safe approach with decrease intraoperative blood loss and similar graft result as compared with open procurement. Further, the team recently presented their 10-year experience and concluded that laparoscopic left lateral sectionectomy could be a possible standard practice for donor hepatectomy (14).
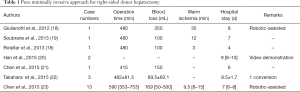
Adult living-related liver transplantation requires a right lobe graft to provide sufficient graft size for the recipient. Although left-sided laparoscopic donor hepatectomy is becoming accepted as a potential beneficial alternative to open left sided donor procurement (15), the efforts to extend the procedure for the right-sided liver donation are much more challenging (16). Following the first laparoscopy-assisted donor right hepatectomy reported in 2006 (17), only a small number of selected donors with favorable anatomy were documented during the evolution of minimally invasive technique in the past decade (Table 1) (19-21). Most reports regarding minimally invasive donor right hepatectomy were either hand-assisted procedure or were with high conversion and complication rates (24).
Full table
Donor safety in MIS right-sided hepatectomy
Donor risk is always the most important consideration with regards to a wider application of living-related liver transplantation. While liver surgeons were beginning their innovative standardization of a left-sided donor procedure, a revolution in the field of right-sided donor hepatectomy was also slowly taking form. Given the MIS right-sided liver donor surgery was generally a combination of advanced techniques in both living donor transplantation and MIS surgery, hybrid surgery, with highly selective cases performed in a pure MIS fashion were carried as the stepping stone. Takahara et al. presented their experience of attempts and evolution for the minimally invasive donor hepatectomy between 2007 and 2013 (22). The series reported 39 laparoscopy-assisted and 6 pure laparoscopy procedures, in which 25 laparoscopy-assisted and 3 pure laparoscopic procedures were performed for right-sided procurement. The procedures were difficult even for the experienced team. In this series, the conversion rate was 16.7% and the complication was 33.3% regarding pure laparoscopic approach.
As illustrated in Table 1, only a few cases of total laparoscopic living donor right hepatectomy were documented in literature review, including Soubrane et al. and Rotellar et al. in 2013 (16,19), Han et al., Chen et al., and Takahara et al. in 2015 (20-22). The reports of these pioneer surgeries confirmed the feasibility of highly selected cases in the hands of experienced MIS surgeons. It is yet unclear the level of benefit of such an MIS approach, and the long-term outcomes regarding donor or graft.
Additionally, in regard to living donor right hepatectomy, biliary complications have been reported as the most common and feared complications (25). To reduce the complication rate, the usual clipping or Hem-o-loc for ligation of hepatic duct usually used in hepatectomy should be avoided during donor procurement. Although such ligation of the hepatic duct facilitates the operation, the procedure would cause the shorting of right hepatic duct stump for reconstruction in recipient. Thus, most transplant surgeons would divide the hepatic duct sharply without clipping, as performed in open cases. The stump of right hepatic duct on donor side shall be closed with running suture. Moreover, considering the long operation time, some studies have reported poor liver regeneration after MIS (26). However, more data regarding donor recovery should be collected for further evaluation.
Robotic approach in donor procurement
Beyond the benefits provided by conventional laparoscopy, the robotic surgical system has been applied to overcome the reduced visualization, restricted range of motion and physiological tremor (27,28) Although the complex vascular and biliary anatomy of liver surgery along with the difficult exposure and risk of bleeding, made for a precipitous learning curve for MIS approaches for liver resection. The robotic surgical system has lowered some of the barriers for adoption of an MIS approach for major hepatectomy (29). Robotic hepatectomy is well documented as safe and feasible (30,31), and the assistance of robotic system allowed more major liver resections (32).
As a pioneer of robotic approach in general surgery, Giulianotti et al. presented the very first case of donor right hepatectomy in 2012 (18). It is not surprising that the robot-assisted system provided the first right-sided donor procedure in advance to the reports of conventional laparoscopic donor procurement. The precise nature of robotic procedures allowed a proper reconstruction of vascular structures, including one large branch of middle hepatic vein at S8. This creative case demonstrated that the detail of the donor procedure is not compromised with a robotic minimally invasive approach. Although a delay portal vein stenosis was noted 6 months later with the possible reason of formation of a band of scar tissue, the donor was fully active with normal liver function after percutaneous trans-hepatic approach for portal vein dilation. This outcome encouraged our entry into minimally invasive donor right hepatectomy.
We initiated a pure MIS donor hepatectomy program after accumulating wide experience of robotic liver resection in 2013. No open conversion occurred in our first 15 consecutive cases, in which 13 donors underwent right hepatectomy. All donors had uneventful perioperative course, except one delayed bile leak after the patient was discharged (23).
Further considerations regarding MIS donor procedure
A longer warm ischemic time during the graft procurement under robotic surgery may adversely affect results of liver transplantation. To limit the warm ischemic time, extension of the umbilical wound and creation of the upper midline wound have been discussed. However, suprapubic wound with Pfannenstiel incision was also proposed for better cosmetic effect. To realize the possible effect of the ischemic time, the recipient outcome regarding the graft function should be carefully evaluated. The graft function shall not be considered as a direct reflection of the ischemic time or donor surgical effect, however, a proper result would ensure the feasibility and effectiveness for MIS donor right hepatectomy.
In minimally invasive liver surgery, the liver donor procedure is more technical demanding when fragile parenchyma is encountered, especially when control of hepatic inflow is avoided to minimize ischemic injury. Standardized steps of donor procurement procedures have been borrowed from hepatectomy procedures. Among them, procedures like hanging maneuver during the open liver surgery should be considered. The maneuver not only guided the posterior transection line with potential bleeding control, but also ensured the meticulous deep parenchyma dissection (33).
In addition to pre-operative magnetic resonance imaging, more than 14% bile duct variation may be detected by intra-operative cholangiography (34). Therefore, real-time fluorescent cholangiography with intravenous indocyanine green could be considered for donor candidates. During MIS, the technique not only provided better delineation of the bile duct anatomy, but also overcomes the limitations of intra-operative cholangiography, including 2-D image and radiation exposure (35).
Anatomic variation is inevitable in liver surgery. However, the anatomy variation encountered frequently that is readily dealt with in open surgery might be a nightmare in an MIS procedure. Nevertheless, the beginning of the development of MIS approach was to recruit more potential donor, and no extra exclusion criteria should be added to the list regarding open candidate. Additionally, although it would extend the operative time, individual handling of the hepatic veins with meticulous hemostasis as well as the possible reconstruction for hepatic veins, and in sequence the proper graft function. The flexibility of robotic system is expected to overcome the limitation of usual MIS approach, however, the potential benefits compared with the conventional laparoscopy shall be carefully evaluated. Further exploring, to recruit more potential living-related liver donors for the demand of graft and the urgency of end stage liver disease, optimizing the postoperative course and limiting abdominal wall injury were expected, especially for the young donors. However, the benefit of robotic procedures shall be assessed beyond the consideration of cosmetic effect. Quantitative data including post-operative pain, post-operative recovery of daily activity and delicate cost-effective studies shall be conducted.
Conclusions
Comparing MIS donor nephrectomy, the application of MIS to donor hepatectomy is fraught with the difficulty due to anatomic variations, and need for parenchymal transection. The robotic surgical system overcomes the reduced visualization, restricted range of motion and physiological tremor associated with laparoscopic surgery (27,36). However, robotic donor right hepatectomy need to be evaluated carefully in experience hands. Nowadays, various approaches have been conducted for the liver donor operation, including smaller incision for laparotomy and conventional laparoscopy. Comparisons with other procedures and assessment for the performance from the standpoint of optimizing the surgical technique and reducing morbidity are required for robotic approach.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Starzl TE. The Current Status of Liver Transplantation. Hosp Pract (Hosp Ed) 1971;6:47-60. [Crossref] [PubMed]
- Wu YM, Ho MC, Hu RH, et al. Liver transplantation for acute hepatic failure. Transplant Proc 2004;36:2226-7. [Crossref] [PubMed]
- Ninomiya M, Shirabe K, Facciuto ME, et al. Comparative study of living and deceased donor liver transplantation as a treatment for hepatocellular carcinoma. J Am Coll Surg 2015;220:297-304.e3. [Crossref] [PubMed]
- Olthoff KM, Abecassis MM, Emond JC, et al. Outcomes of adult living donor liver transplantation: comparison of the Adult-to-adult Living Donor Liver Transplantation Cohort Study and the national experience. Liver Transpl 2011;17:789-97. [Crossref] [PubMed]
- Chan SC, Fan ST, Lo CM, et al. A decade of right liver adult-to-adult living donor liver transplantation: the recipient mid-term outcomes. Ann Surg 2008;248:411-9. [PubMed]
- Lo CM, Fan ST, Liu CL, et al. Adult-to-adult living donor liver transplantation using extended right lobe grafts. Ann Surg 1997;226:261-9; discussion 269-70. [Crossref] [PubMed]
- Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg 2009;250:831-41. [Crossref] [PubMed]
- Dagher I, Gayet B, Tzanis D, et al. International experience for laparoscopic major liver resection. J Hepatobiliary Pancreat Sci 2014;21:732-6. [Crossref] [PubMed]
- Kim SH, Kim YK. Improving outcomes of living-donor right hepatectomy. The Br J Surg 2013;100:528-34. [Crossref] [PubMed]
- Abecassis MM, Fisher RA, Olthoff KM, et al. Complications of living donor hepatic lobectomy--a comprehensive report. Am J Transplant 2012;12:1208-17. [Crossref] [PubMed]
- Cherqui D, Soubrane O, Husson E, et al. Laparoscopic living donor hepatectomy for liver transplantation in children. Lancet 2002;359:392-6. [Crossref] [PubMed]
- Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825-30. [Crossref] [PubMed]
- Soubrane O, Cherqui D, Scatton O, et al. Laparoscopic left lateral sectionectomy in living donors: safety and reproducibility of the technique in a single center. Ann Surg 2006;244:815-20. [Crossref] [PubMed]
- Soubrane O, de Rougemont O, Kim KH, et al. Laparoscopic Living Donor Left Lateral Sectionectomy: A New Standard Practice for Donor Hepatectomy. Ann Surg 2015;262:757-61; discussion 761-3. [Crossref] [PubMed]
- Samstein B, Griesemer A, Cherqui D, et al. Fully laparoscopic left-sided donor hepatectomy is safe and associated with shorter hospital stay and earlier return to work: A comparative study. Liver Transpl 2015;21:768-73. [Crossref] [PubMed]
- Rotellar F, Pardo F, Benito A, et al. Totally laparoscopic right-lobe hepatectomy for adult living donor liver transplantation: useful strategies to enhance safety. Am J Transplant 2013;13:3269-73. [Crossref] [PubMed]
- Koffron AJ, Kung R, Baker T, et al. Laparoscopic-assisted right lobe donor hepatectomy. Am J Transplant 2006;6:2522-5. [Crossref] [PubMed]
- Giulianotti PC, Tzvetanov I, Jeon H, et al. Robot-assisted right lobe donor hepatectomy. Transpl Int 2012;25:e5-9. [Crossref] [PubMed]
- Soubrane O, Perdigao Cotta F, Scatton O. Pure laparoscopic right hepatectomy in a living donor. Am J Transplant 2013;13:2467-71. [Crossref] [PubMed]
- Han HS, Cho JY, Yoon YS, et al. Total laparoscopic living donor right hepatectomy. Surg Endosc 2015;29:184. [Crossref] [PubMed]
- Chen KH, Huang CC, Siow TF, et al. Totally laparoscopic living donor right hepatectomy in a donor with trifurcation of bile duct. Asian J Surg 2016;39:51-5. [Crossref] [PubMed]
- Takahara T, Wakabayashi G, Hasegawa Y, et al. Minimally invasive donor hepatectomy: evolution from hybrid to pure laparoscopic techniques. Ann Surg 2015;261:e3-4. [Crossref] [PubMed]
- Chen PD, Wu CY, Hu RH, et al. Robotic liver donor right hepatectomy: A pure, minimally invasive approach. Liver Transpl 2016;22:1509-18. [Crossref] [PubMed]
- Park JI, Kim KH, Lee SG. Laparoscopic living donor hepatectomy: a review of current status. J Hepatobiliary Pancreat Sci 2015;22:779-88. [Crossref] [PubMed]
- Iida T, Ogura Y, Oike F, et al. Surgery-related morbidity in living donors for liver transplantation. Transplantation 2010;89:1276-82. [Crossref] [PubMed]
- Komori Y, Iwashita Y, Ohta M, et al. Effects of different pressure levels of CO2 pneumoperitoneum on liver regeneration after liver resection in a rat model. Surg Endosc 2014;28:2466-73. [Crossref] [PubMed]
- Giulianotti PC, Coratti A, Angelini M, et al. Robotics in general surgery: personal experience in a large community hospital. Arch Surg 2003;138:777-84. [Crossref] [PubMed]
- Liang JT, Lai HS. Surgical technique of robotic D3 lymph node dissection around the inferior mesenteric artery with preservation of the left colic artery and autonomic nerves for the treatment of distal rectal cancer. Surg Endosc 2014;28:1727-33. [Crossref] [PubMed]
- Tsung A, Geller DA, Sukato DC, et al. Robotic versus laparoscopic hepatectomy: a matched comparison. Ann Surg 2014;259:549-55. [Crossref] [PubMed]
- Montalti R, Patriti A, Troisi RI. Robotic Versus Laparoscopic Hepatectomy: What Is the Best Minimally Invasive Approach? Ann Surg 2015;262:e70. [Crossref] [PubMed]
- Lai EC, Yang GP, Tang CN. Robot-assisted laparoscopic liver resection for hepatocellular carcinoma: short-term outcome. Am J Surg 2013;205:697-702. [Crossref] [PubMed]
- Wu YM, Hu RH, Lai HS, et al. Robotic-assisted minimally invasive liver resection. Asian J Surg 2014;37:53-7. [Crossref] [PubMed]
- Vennarecci G, Levi Sandri GB, Ettorre GM. Performing the ALPPS Procedure by Anterior Approach and Liver Hanging Maneuver. Ann Surg 2016;263:e11. [Crossref] [PubMed]
- Ran S, Wen TF, Yan LN, et al. Risks faced by donors of right lobe for living donor liver transplantation. Hepatobiliary Pancreat Dis Int 2009;8:581-5. [PubMed]
- Pesce A, Piccolo G, La Greca G, et al. Utility of fluorescent cholangiography during laparoscopic cholecystectomy: A systematic review. World J Gastroenterol 2015;21:7877-83. [Crossref] [PubMed]
- Lee SY, Allen PJ, Sadot E, et al. Distal pancreatectomy: a single institution's experience in open, laparoscopic, and robotic approaches. J Am Coll Surg 2015;220:18-27. [Crossref] [PubMed]


