Congenital membranous occlusion of the suprahepatic inferior vena cava in a pediatric liver transplant
Introduction
Membranous occlusion of the suprahepatic inferior vena cava (IVC), also known as obliterative hepatocavopathy, is a rare, obstructive lesion of the cava, resulting in hepatic venous outflow obstruction and centrilobular hepatic congestion. Rare cases are reported in children (1). Two etiologies of the lesion have been postulated—congenital vascular malformation or the consequence of organized thrombus within the IVC (2). We report a case of congenital suprahepatic caval occlusion, discovered in a 2-year-old female after two liver transplantations.
Case presentation
The patient was a 2-year-old African-American female with multiple medical comorbidities, including, but not limited to, end-stage liver disease secondary to neonatal hepatitis of unknown etiology. She underwent orthotopic liver transplant; however, at the time of transplant, the liver had very poor reperfusion. Areas of infarction were demonstrated on biopsies collected on post-transplantation day two and the patient subsequently became febrile. Duplex ultrasonography and abdominal CT scan were performed and both studies revealed hepatic artery thrombosis (HAT). She was listed as status 1A for HAT and received her second cadaveric liver transplant on post-operative day 16 for which she required an iliac artery conduit for hepatic artery inflow. Her second transplantation was immediately complicated by repeat HAT, necessitating an emergent return to the operating room for thrombectomy of the iliac artery conduit and implantation of a hepatic artery Doppler. Post-operative ultrasound revealed patency of all vessels.
Interval CT scan performed to evaluate progressive ascites, abdominal tenderness, and persistent fevers, demonstrated enlargement of the liver with inhomogeneous perfusion as well as abnormal flow in the hepatic artery. Hepatic duplex performed revealed decreased flow in the hepatic artery compared to prior imaging. An IR liver biopsy was requested; however, inability to traverse a wire into the IVC lead to performance of an IVC venogram which revealed patent hepatic veins with occlusion of the suprahepatic IVC. Contrast flow to the right atrium was demonstrated via several collaterals from the azygos system (free hepatic vein/IVC pressure =17 mmHg; RA pressure =3 mmHg).
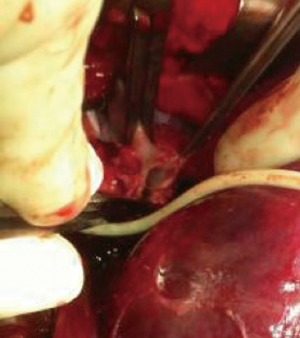
Since there was inability to cross the IVC, the patient was taken to the operating room where patency of the suprahepatic venous anastomosis was noted. Unfortunately, complete endothelialization of the IVC just above the level of the diaphragm was discovered (Figure 1). After complete vascular exclusion, she underwent reconstruction of her suprahepatic IVC to the intrapericardial IVC using an end-to-side technique after complete mobilization of the liver. Following this, clamps were removed and the liver was reperfused with normal flow through the hepatic artery, portal vein, and hepatic veins on ultrasound. Intraoperative venogram demonstrated the patency of the new anastomosis with filling of the right atrium via the IVC. The patient eventually was discharged with excellent liver function.
Discussion
Congenital membranous occlusion of the IVC is a rare anomaly attributed to vascular malformation during fetal development. The embryogenesis of the suprahepatic IVC is an intricate process. During the fourth week of fetal life, channels in the embryonic sinusoidal network drain blood from the vitelline, umbilical, and right subcardinal veins (2,3). The proximal portion of the early right vitelline vein becomes a common drainage outlet into the sinus venosus, which eventually forms the suprahepatic and intrahepatic IVC (3,4). The ductus venosus then drains blood from the left umbilical vein and directs it into the common drainage outlet. Abnormal persistence or regression of these sinusoidal channels may result in failure of establishment of right atrial inflow from the sinus venosus or extension of the normal obliterative process of the ductus venosus into the IVC (2).
Physical exam reveals signs of hepatic venous congestion. Adults with chronic membranous occlusion of the IVC will often display large truncal collateral vessels with cephalad flow (2,5). Diagnosis is confirmed with inferior vena cavography which demonstrates complete occlusion of the IVC at the junction of the right atrium (3). Patent hepatic veins with several collaterals communicating between the hepatic and hemiazygos systems are also demonstrated (1,3). The azygos vein is often markedly dilated. Initial attempts at treatment should consist of balloon angioplasty or transatrial membranotomy (1). Should these efforts be impossible, more complex vena caval and portal decompressive surgery is warranted to prevent chronic obstruction and the sequelae of severe centrilobular fibrosis (2).
Unfortunately, this child lost her initial graft due to HAT, which was related to unrecognized outflow obstruction. This case of congenital membranous occlusion of the IVC nearly resulted in a second graft loss but an aggressive attempt at intraoperative evaluation of the suprahepatic IVC revealed obliteration of the lumen. Thankfully, reconstruction was possible and the inflow was restored leading to a fully functional graft. In conclusion, this case demonstrates unrecognized congenital membranous occlusion of the IVC and imparts that one must evaluate early and aggressively for outflow occlusion in the setting of unexplained inflow compromise in liver transplantation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient’s guardian for publication of this manuscript and any accompanying images.
References
- Gandhi SK, Pigula FA. Congenital membranous obstruction of the inferior vena cava. Ann Thorac Surg 2004;78:1849. [Crossref] [PubMed]
- Kew MC, Hodkinson HJ. Membranous obstruction of the inferior vena cava and its causal relation to hepatocellular carcinoma. Liver Int 2006;26:1-7. [Crossref] [PubMed]
- Kandpal H, Sharma R, Gamangatti S, et al. Imaging the inferior vena cava: a road less traveled. Radiographics 2008;28:669-89. [Crossref] [PubMed]
- Cossu ML, Ruggiu M, Fais E, et al. Congenital anomalies of the inferior vena cava. Minerva Chir 2000;55:703-8. [PubMed]
- Fukuda A, Ogura Y, Kanazawa H, et al. Living donor liver transplantation for Budd-Chiari syndrome with hepatic inferior vena cava obstruction after open pericardial procedures. Surg Today 2013;43:1180-4. [Crossref] [PubMed]