Comments on “JAMA PATIENT PAGE. Treatment of Liver Cancer”
Hepatocellular carcinoma (HCC), which originates from the hepatocyte, and metastatic liver cancer, which happens in a different part of the body and metastasizes to the liver, occupy the majority of liver cancer. HCC, which accounts for 90% of liver cancers, is the third leading cause of cancer-related death worldwide (1), and causes an approximated 700,000 deaths worldwide annually (2). HCC occurs in chronic liver inflammation caused by hepatitis B, hepatitis C, ethanol consumption, aflatoxin, non-alcoholic fatty liver disease, autoimmune hepatitis and other chronic liver diseases (3). With the continuous improvement of medical treatment, the diagnosis and treatment of liver cancer are constantly changing.
Currently, optimal treatment for HCC mainly depends on the stage of cancer. Surgical resection and liver transplantation are the sole curative options for the treatment of HCC, especially for early-stage HCC. Although curative surgical therapies have a high 5-year survival rate, there is a significant difference between early-stage and advanced-stage HCC (4). Advanced early surveillance technology has improved the life of patients diagnosed at an early stage, however, most patients are diagnosed with late stage of HCC, and do not meet selection criteria. Furthermore, HCC patients do not show improved long-term disease-free survival or overall survival after surgical resection and auxiliary medication treatment (5-7). On the basis of early surveillance technology and multiple treatment options, how to select the appropriate treatment for different patients is particularly important.
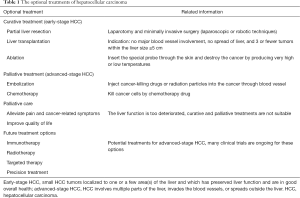
In their summative study, Mokdad and co-workers overview the treatment options of HCC (8). Optimal treatment requires the cooperation of surgeon, oncologist, hepatologist, interventional radiologist, and palliative care specialist. A perfect treatment option needs to consider a variety of factors including the stage of cancer, the underlying function of the liver, and the overall health of the patient. Curative and palliative treatments could be selected when the liver function is suitable. At present, multiple options are available for early-stage and advanced-stage HCC (8) (Table 1). For early-stage HCC, 5-year survival rate is similar among partial liver resection, liver transplantation, and ablation, approximate 70% in most studies. Partial liver resection is perfect treatment for resectable HCC, because the remnant liver has a strong regenerative ability. Liver transplantation is ideal therapy, and has a lower recurrence rate than liver resection and ablation. For advanced-stage HCC, liver cancer becomes incurable and the objective of these cases is aimed at prolonging life. Chemotherapy is a kind of treatment for non-surgical management of HCC, and sorafenib is the sole systemic agent that has shown a survival benefit for advanced-stage HCC (9). For some advanced-stage HCC, liver function is too deteriorated, and not suitable for curative and palliative treatments. Palliative care emphasizes to alleviate pain and improve quality of life.
Full table
Many other therapies, called future treatment options, are being studied in clinical trials for HCC, especially for advanced-stage HCC. Future treatment options include immunotherapy, radiotherapy, targeted therapy, and precision treatment (Table 1). Chronic liver inflammation is a major risk factor for the development and progression of HCC, and the tumor-induced antitumor immunity plays a key role in the prognosis of HCC. Therefore, HCC immunological research can help to understand the immunological mechanism of cancer progression, and explore new strategies for immunotherapy. The application of radiotherapy liver cancer is limited, and generally used as selective treatment after liver resection and ablation. Recent advances in high throughput sequencing technology have helped provide deeper insights into the genomic and transcriptome landscape in HCC (10). With the development of gene sequencing, one-to-one therapy model, named precision treatment, appears. Increasing numbers of molecular targeted gene changes have been found in occurrence of HCC, and been applied in the treatment of HCC (11). Precision treatment will be an indispensable and significant option for advanced-stage HCC.
However, some defects still exist in future treatment options in HCC. Firstly, most patients in the advanced-stage HCC exhibit a low sensitivity for radiotherapy and chemotherapy (12). Secondly, drug resistance hampers the clinical application of targeted therapy in the treatment of advanced-stage HCC (13). Lastly, the diversity and complexity of genetic change exists in HCC, but many drugs or studies for targeted therapy and precision treatment only focus on the part of them. These will bring a huge challenge in targeted therapy and precision treatment of HCC.
Since mono-treatment has a poor effect for HCC, we could strengthen the treatment efficacy by combining different therapy methods. The different types of combination with curative treatment, palliative treatment, and future treatment options will bring unexpected treatment effects. This needs further considerable research. In consideration of the complexity of liver cancer, multi-disciplinary cooperation is still an important direction for the treatment of liver cancer in future. As is well-known, optimal treatment requires multi-disciplinary cooperation. But in the past, surgeon, oncologist, pathologist and hepatologist are the main role of multi-disciplinary cooperation. With the application of targeted therapy and precision treatment in cancer therapy, bioinformatics scientist plays an important role in analysis and decision process, and should join the multidisciplinary cooperation to make an optimal treatment. This article expounds existing liver cancer treatment and advances our thinking for new treatment in the future.
Acknowledgements
Funding: The authors acknowledge grant support of International Science and Technology Cooperation Projects (No. 2015DFA30650 and No. 2010DFB33720); Capital Special Research Project for Health Development (No. 2014-2-4012); Capital Research Project for Characteristics Clinical Application (No. Z151100004015170); and Program for New Century Excellent Talents in University (No. NCET-11-0288).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet 2016;387:251-72. [Crossref] [PubMed]
- Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69-90. [Crossref] [PubMed]
- El-Serag HB. Hepatocellular carcinoma. N Engl J Med 2011;365:1118-27. [Crossref] [PubMed]
- Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996;334:693-9. [Crossref] [PubMed]
- Kamiyama T, Nakanishi K, Yokoo H, et al. Recurrence patterns after hepatectomy of hepatocellular carcinoma: implication of Milan criteria utilization. Ann Surg Oncol 2009;16:1560-71. [Crossref] [PubMed]
- Eggert T, McGlynn KA, Duffy A, et al. Epidemiology of fibrolamellar hepatocellular carcinoma in the USA, 2000-10. Gut 2013;62:1667-8. [Crossref] [PubMed]
- Ye QH, Qin LX, Forgues M, et al. Predicting hepatitis B virus-positive metastatic hepatocellular carcinomas using gene expression profiling and supervised machine learning. Nat Med 2003;9:416-23. [Crossref] [PubMed]
- Mokdad AA, Singal AG, Yopp AC. JAMA PATIENT PAGE. Treatment of Liver Cancer. JAMA 2016;315:100. [Crossref] [PubMed]
- Llovet JM, Ricci S, Mazzaferro V, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008;359:378-90. [Crossref] [PubMed]
- Shibata T, Aburatani H. Exploration of liver cancer genomes. Nat Rev Gastroenterol Hepatol 2014;11:340-9. [Crossref] [PubMed]
- Llovet JM, Villanueva A, Lachenmayer A, et al. Advances in targeted therapies for hepatocellular carcinoma in the genomic era. Nat Rev Clin Oncol 2015;12:408-24. [Crossref] [PubMed]
- Lau CK, Yang ZF, Fan ST. Role of stem cells in normal liver and cancer. Anticancer Agents Med Chem 2011;11:522-8. [Crossref] [PubMed]
- Llovet JM, Bruix J. Molecular targeted therapies in hepatocellular carcinoma. Hepatology 2008;48:1312-27. [Crossref] [PubMed]


