Conservative and surgical management of pancreatic trauma in adult patients
Introduction
The pancreas is an organ located deep in the abdominal cavity, whose anatomical relationship with the digestive and vascular structures (1-4) explains the complexity and severity of pancreatic trauma which represents less than 5% of abdominal trauma (5,6). Pancreatic trauma is potentially lethal when combined with duodenal perforation or closely related arterial bleeding (2,7). These injuries remain difficult to diagnose and undeniably pose a problem in therapeutic strategy. An abdominal computer tomography (CT) allows diagnosis and severity assessments of pancreatic trauma, presence of pancreatic duct injury or associated bleeding (8-11). A delay in diagnosis or underestimation of its severity may be responsible for serious complications such as intra-abdominal bleeding, pancreatic fistula or intra-abdominal collections (12-14). The aim of this retrospective study was to report our single-center experience in the management and treatment of pancreatic trauma.
Methods
Patients
All patients hospitalized for pancreatic trauma in the Digestive Surgery Service, Hepatobiliary, Pancreatic and Liver Transplantation at the Henri Mondor University Hospital (Créteil, France) were identified from the Programme de Médicalisation des Systèmes d’Information database (PMSI) between 2005 and 2013. Data from the PMSI were the dates, the main diagnosis, associated diagnosis, age and sex of the patients. All standardized summaries on PMSI whose code belonging to the categories of the International Classification of Diseases, 10th Revision (ICD-10), in connection with abdominal and pancreatic trauma or associated diagnosis were selected.
Classification of traumatic injury of the pancreas according to the American Association for Surgery of Trauma (AAST) (15)
- Grade 1: minor contusion without ductal injury;
- Grade 2: major contusion/laceration without ductal injury or tissue loss;
- Grade 3: distal transection or parenchymal injury with ductal injury;
- Grade 4: proximal transection or parenchymal injury involving ampulla;
- Grade 5: mass destruction of the pancreatic head.
Management of traumatic injury of the pancreas
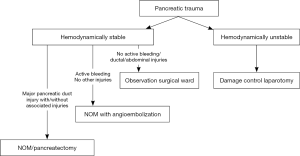
The first step is to comprehend that we are dealing with a trauma patient and usually not just an isolated pancreatic injury. The management directly correlated to other variable besides the injured pancreas itself, including the patient’s hemodynamic status, presence and severity of associated injuries such as cranial, chest, pelvic and extremities, and hypothermia. Different patients with more or less same grade of pancreatic injury can have different management as shown in Figure 1.
Statistical analysis
Quantitative variables were expressed as mean ± standard deviation. The qualitative variables are expressed as a percentage. As it is not homogenous groups we mainly used simple descriptive statistics.
Results
Baseline characteristics
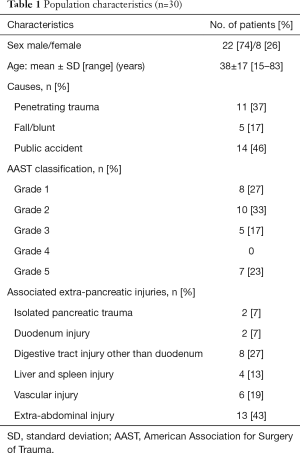
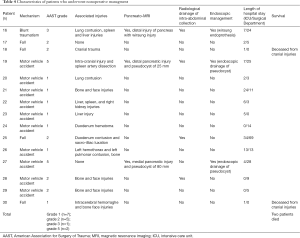
Thirty patients with pancreatic trauma (11.5% of all abdominal injuries) were hospitalized in our department between 2005 and 2013. The majority of them were male (74%) and the average age was 38±17 years (15–83 years). The general characteristics of the study population are described in Table 1.
Full table
Mechanisms and localization of pancreatic trauma
More than half (63%, n=19) of pancreatic trauma were blunt, and they occurred due to motor vehicle accident in 46% of the cases (n=14) or after fall/crushing in 17% of the cases (n=5). In 37% of patients (n=11), penetrating trauma (stab/gunshot wound) was the cause of the pancreatic injury. As for the location of the trauma within the pancreas it was located at the head in 11, body in 7 and tail of the pancreas in 9 patients. The injury was located at the junction body-tail in two cases and one case at the junction between the head and body.
Hemodynamic state on arrival and injuries
Fifteen patients (50%) were hemodynamically unstable upon arrival and needed an emergency laparotomy. Of these patients, 2 had severe hemorrhage accompanied by hypovolemic shock. The other 13 patients were operated due to penetrating trauma with hemodynamically instability. Thirteen (43%) of the total number of patients had extra-abdominal injuries such as brain, chest and pelvic. Eight patients (27%) had associated hollow organ injury.
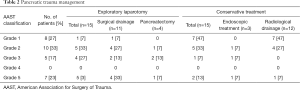
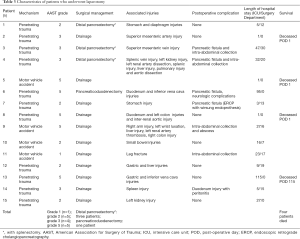
Characteristics of patients who underwent exploratory laparotomy (n=15)
The diagnosis of pancreatic injury was made during the exploratory laparotomy in 10 patients. Diagnosis of pancreatic injury was done by the preoperative CT scan in 5 patients. Pancreatic resection was performed in 4 patients: 3 patients had distal pancreatectomy with splenectomy and 1 patient had pancreaticoduodenectomy for pancreatic injury grade 5. The other 11 patients had a wide peri-pancreatic surgical drainage (Tables 2,3).
Full table
Full table
Postoperative mortality and morbidity following laparotomy
Among the patients operated, 4 died, 3 of them within 24 hours of admission, and the fourth patient after 115 days of hospitalization. Eight (8/15, 53%) patients had a postoperative complication (Table 3). From the 4 patients who had pancreatectomy, 3 patients (75%) had pancreatic fistula. Five patients had intra-abdominal collection that required radiological drainage. One patient had peritonitis due to perforated duodenal ulcer and needed reoperation. One patient suffered from pneumonia and polyneuropathy.
Characteristic of patients who underwent nonoperative management (NOM)
Fifteen (50%) patients underwent NOM (Table 4). Twelve patients initially needed intensive care unit (ICU) supervision with a mean stay of 13±12 days. The other three patients were hospitalized in our surgical ward with a mean stay of 9±4.5 days. Monitoring CT scan on the 7th day of hospitalization did not find any abdominal fluid collection in 10 patients. Two patients died within 24 hours of admission due to associated severe head injury. In one patient sphincterotomy and stenting of the pancreatic duct was performed.
Full table
Long-term survival of patients
The average hospital stay was 28.9±23.4 days (range, 1–115 days). Overall mortality was 20% (n=6). Among the 24 surviving patients, 2 patients developed pancreatic pseudocyst and were drained by endoscopy, and 2 patients had atrophy of the pancreatic gland correlated to the old contusion site.
Discussion
This retrospective study shows that the prevalence of pancreatic trauma among all abdominal trauma patients hospitalized in our department was 11.5% with an overall mortality of 20%. Pancreatic injuries were mostly blunt trauma (63%) and the etiology was dominated by motor vehicle accident in 46% of the cases, followed by stab wounds in 37% and falls or crushing in 17% of the cases. The incidence of pancreatic trauma is greater than reported in the literature which stands between 3–5% (16), an explanation to that is by the relatively small size of our series and the fact that not all abdominal trauma were hospitalized in our department. The average age of patients is 38 years old, which does not differ from other published series where the age is less than 40 years in 80% of the cases, in addition 74% of patients in our series are males, as well correspond to the literature data (1,17,18). Isolated pancreatic trauma is rarely the case, as this study shows that in 90% of the patients other associated injuries were treated. This is not the case for pancreatic injuries occurring in children which are often isolated (sports injuries or bike fall). The main causes of pancreatic trauma in this series were motor vehicle accident and stab wounds, unlike data from the United States where the main cause of pancreatic trauma is penetrating (firearms and knives) (1,3,19-21). The reason is probably due to much stricter legislation regarding firearms in Europe where most pancreatic trauma are blunt ones and the most frequent mechanisms are linked to acceleration-deceleration or abdominal contusion to the driver from steering wheel (2,22). In this study 21 patients had a full body CT scan, only 1 patient had a CT scan that was consider normal, a false negative rate of 5% which is lower than the data reported in the literature (40%) (8). Also in our series, the diagnosis of pancreatic injury was made by magnetic resonance imaging (MRI) (3 patients), however access to MRI in emergency setting and its yield is under evaluation (23,24).
The decision to perform pancreatectomy in the setting of trauma is still a pending question. The majority of patients who were operated in our series (n=11/15) had a peri-pancreatic drainage, except 4 patients who had pancreatectomy (distal n=3, head n=1). As for pancreatic injury grades 1 and 2, the NOM is the most effective as long as there is no involvement of the main pancreatic duct. This strategy is effective since morbidity is less than 20% and mortality is relatively low (20,25). This is in accordance with our results which show that 80% (12/15) were successfully treated with this strategy. As for grade 3 and 4 pancreatic injury, distal pancreatectomy or surgical drainage are the indication of choice for body-tail contused areas associated with distal pancreatic duct injury (1,25). Distal pancreatectomy is often preferred over drainage because it decreases mortality and the risk of operative complications (1,20,26). In case of complete traumatic transection of the pancreatic neck (i.e., pancreaticojejunostomy of the distal stump and sutured of the cephalic stump) may be suggested. In our series, 5 patients had pancreatic injury grade 3, of whom 2 patients had distal pancreatectomy, 2 patients had surgical drainage and 1 patient was not operated and a stent was placed within the wirsung duct via endoscopic retrograde cholangiopancreatography (ERCP). The objective of ERCP is twofold: to confirm the diagnosis of pancreatic duct injury and to insert a bridge prosthesis over the contused area (27). A therapeutic alternative is to perform only sphincterotomy which aims to reduce the rate of pancreatic fistula by reducing the intra-ductal pressure (28). For pancreatic injury grade 5 there are several possibilities varies from NOM to surgical drainage and up to pancreaticoduodenectomy. The published data favor NOM with satisfactory results (19,25), even in cases of duodenal or bile duct injuries (29). Pancreaticoduodenectomy is associated with high mortality rate (45%) while more conservative approach has much lower mortality rate of 22–25% (29-31). Some authors have described the possibility to perform pancreaticoduodenectomy in two steps with a reconstruction 24 to 48 hours later (32). In our study the majority of patients (n=5/7) with grade 5 injury underwent surgical drainage, with a mortality rate of 43% (n=3/7), though two patients died within 24 hours due to associated injuries and probably not from the pancreatic injury itself.
The mortality of the NOM group was 13% (2/15) which is higher than reported in the literature. When NOM is decided, it includes: resuscitation, analgesia, parenteral nutrition and monitoring in surgical ward, similar in many ways to the treatment in case of acute pancreatitis. The issue of antibiotics or octreotide treatment in the nonoperative group is still controversial (33).
The limitations of this study include its retrospective nature and the limited sample size. It is difficult to draw any robust conclusions from comparison of the two groups since it is not homogeneous groups.
In conclusion, operative management of pancreatic trauma leads to a higher mortality, but this must not be necessarily related to the pancreas injury alone but also to the associated injuries including liver, spleen and vascular trauma which may cause impaired outcome more than pancreas injury.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the local committee.
References
- Cogbill TH, Moore EE, Morris JA Jr, et al. Distal pancreatectomy for trauma: a multicenter experience. J Trauma 1991;31:1600-6. [Crossref] [PubMed]
- Heuer M, Hussmann B, Lefering R, et al. Pancreatic injury in 284 patients with severe abdominal trauma: outcome, course, and treatment algorithm. Langenbecks Arch Surg 2011;396:1067-76. [Crossref] [PubMed]
- Jones RC. Management of pancreatic trauma. Am J Surg 1985;150:698-704. [Crossref] [PubMed]
- Krige JE, Kotze UK, Hameed M, et al. Pancreatic injuries after blunt abdominal trauma: an analysis of 110 patients treated at a level 1 trauma centre. S Afr J Surg 2011;49:58-60, 62-4 passim. [PubMed]
- Chinnery GE, Krige JE, Kotze UK, et al. Surgical management and outcome of civilian gunshot injuries to the pancreas. Br J Surg 2012;99 Suppl 1:140-8. [Crossref] [PubMed]
- Lahiri R, Bhattacharya S. Pancreatic trauma. Ann R Coll Surg Engl 2013;95:241-5. [Crossref] [PubMed]
- Wang GF, Li YS, Li JS. Damage control surgery for severe pancreatic trauma. Hepatobiliary Pancreat Dis Int 2007;6:569-71. [PubMed]
- Bradley EL 3rd, Young PR Jr, Chang MC, et al. Diagnosis and initial management of blunt pancreatic trauma: guidelines from a multiinstitutional review. Ann Surg 1998;227:861-9. [Crossref] [PubMed]
- Ilahi O, Bochicchio GV, Scalea TM. Efficacy of computed tomography in the diagnosis of pancreatic injury in adult blunt trauma patients: a single-institutional study. Am Surg 2002;68:704-7; discussion 707-8. [PubMed]
- Phelan HA, Velmahos GC, Jurkovich GJ, et al. An evaluation of multidetector computed tomography in detecting pancreatic injury: results of a multicenter AAST study. J Trauma 2009;66:641-6; discussion 646-7. [Crossref] [PubMed]
- Tyburski JG, Dente CJ, Wilson RF, et al. Infectious complications following duodenal and/or pancreatic trauma. Am Surg 2001;67:227-30; discussion 230-1. [PubMed]
- Biffl WL, Moore EE, Croce M, et al. Western Trauma Association critical decisions in trauma: management of pancreatic injuries. J Trauma Acute Care Surg 2013;75:941-6. [Crossref] [PubMed]
- Krige JE, Beningfield SJ, Nicol AJ, et al. The management of complex pancreatic injuries. S Afr J Surg 2005;43:92-102. [PubMed]
- Lin BC, Chen RJ, Fang JF, et al. Management of blunt major pancreatic injury. J Trauma 2004;56:774-8. [Crossref] [PubMed]
- Moore EE, Cogbill TH, Malangoni MA, et al. Organ injury scaling, II: Pancreas, duodenum, small bowel, colon, and rectum. J Trauma 1990;30:1427-9. [Crossref] [PubMed]
- Pata G, Casella C, Di Betta E, et al. Extension of nonoperative management of blunt pancreatic trauma to include grade III injuries: a safety analysis. World J Surg 2009;33:1611-7. [Crossref] [PubMed]
- Akhrass R, Yaffe MB, Brandt CP, et al. Pancreatic trauma: a ten-year multi-institutional experience. Am Surg 1997;63:598-604. [PubMed]
- Vasquez JC, Coimbra R, Hoyt DB, et al. Management of penetrating pancreatic trauma: an 11-year experience of a level-1 trauma center. Injury 2001;32:753-9. [Crossref] [PubMed]
- Patton JH Jr, Lyden SP, Croce MA, et al. Pancreatic trauma: a simplified management guideline. J Trauma 1997;43:234-9; discussion 239-41. [Crossref] [PubMed]
- Smego DR, Richardson JD, Flint LM. Determinants of outcome in pancreatic trauma. J Trauma 1985;25:771-6. [Crossref] [PubMed]
- Wisner DH, Wold RL, Frey CF. Diagnosis and treatment of pancreatic injuries. An analysis of management principles. Arch Surg 1990;125:1109-13. [Crossref] [PubMed]
- Leppäniemi A, Haapiainen R, Kiviluoto T, et al. Pancreatic trauma: acute and late manifestations. Br J Surg 1988;75:165-7. [Crossref] [PubMed]
- Fulcher AS, Turner MA, Yelon JA, et al. Magnetic resonance cholangiopancreatography (MRCP) in the assessment of pancreatic duct trauma and its sequelae: preliminary findings. J Trauma 2000;48:1001-7. [Crossref] [PubMed]
- Nirula R, Velmahos GC, Demetriades D. Magnetic resonance cholangiopancreatography in pancreatic trauma: a new diagnostic modality? J Trauma 1999;47:585-7. [Crossref] [PubMed]
- Sharpe JP, Magnotti LJ, Weinberg JA, et al. Impact of a defined management algorithm on outcome after traumatic pancreatic injury. J Trauma Acute Care Surg 2012;72:100-5. [Crossref] [PubMed]
- Wilson RH, Moorehead RJ. Current management of trauma to the pancreas. Br J Surg 1991;78:1196-202. [Crossref] [PubMed]
- Telford JJ, Farrell JJ, Saltzman JR, et al. Pancreatic stent placement for duct disruption. Gastrointest Endosc 2002;56:18-24. [Crossref] [PubMed]
- Wind P, Tiret E, Cunningham C, et al. Contribution of endoscopic retrograde pancreatography in management of complications following distal pancreatic trauma. Am Surg 1999;65:777-83. [PubMed]
- Feliciano DV, Martin TD, Cruse PA, et al. Management of combined pancreatoduodenal injuries. Ann Surg 1987;205:673-80. [Crossref] [PubMed]
- Mansour MA, Moore JB, Moore EE, et al. Conservative management of combined pancreatoduodenal injuries. Am J Surg 1989;158:531-5. [Crossref] [PubMed]
- Strobel O, Schneider L, Philipp S, et al. Emergency pancreatic surgery--demanding and dangerous. Langenbecks Arch Surg 2015;400:837-41. [Crossref] [PubMed]
- Degiannis E, Boffard K. Duodenal injuries. Br J Surg 2000;87:1473-9. [Crossref] [PubMed]
- Amirata E, Livingston DH, Elcavage J. Octreotide acetate decreases pancreatic complications after pancreatic trauma. Am J Surg 1994;168:345-7. [Crossref] [PubMed]