Laparoscopic and robotic approach for hepatocellular carcinoma—state of the art
Introduction
Hepatocellular carcinoma (HCC) is the sixth most common malignant tumor worldwide and the most common primary liver cancer, in over 80% of cases HCC grown on a cirrhotic liver (1,2). Possible curative treatments are liver resection (LR), liver transplantation (LT), and local ablation (3). Since the first reported laparoscopic hepatectomy in 1993, minimally invasive surgical technique in liver surgery has continuously developed. Laparoscopic liver resection (LLR) is now worldwide accepted considering the excellent results shown. Minimally invasive surgical approach for HCC is increasing continuously and in specialized centers seems to become the first-line approach for those patients (2-4). This review presents and discusses state of the art in the laparoscopic and robotic surgical treatment of HCC.
Methods
An electronic search was performed to identify all studies dealing with HCC resected with laparoscopy or robotic approach.
The PubMed/MEDLINE database on December 2015 was searched. The search strategy was (“laparoscopic” OR “robotic”) AND (“hepatocellular carcinoma” OR “hcc”). We found over 600 papers, all study typologies, including case reports and small series were considered if the articles report some new techniques or strategies for HCC resection. We resumed all reported cohort of more than 50 LLR for HCC in Table 1, and the robotic cases are resumed in Table 2.
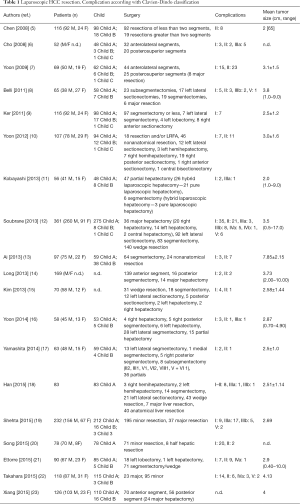
Full table
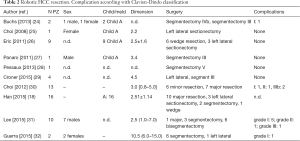
Full table
Laparoscopic approach
Before Louisville
Initially, the experience of LLR was restricted to benign pathologies, and peripheral lesions/left lateral sectionectomy. Since the first LLR, surgical teams consider non-compensated cirrhosis as a contraindication for LR and thereby for LLR (12,33,34). Nonetheless, Ettorre et al. compared LLR (38 were HCC) in two groups with underlined liver disease and normal liver, without detecting differences in terms of morbidity and mortality risks (4). For the first experiences reported, most cases in the laparoscopic group were segmentectomies or subsegmentectomies located in segments II, III, IV, V, or VI (or anterior segment). Since the beginning of 2000 years LLR increased in many centers worldwide. Also, tumor size, type, and location are important in determining indications for LLR for HCC (35,36).
First consensus conference
Considering the worldwide procedures were increasing, the first international consensus conference on LLR was held in 2008 in Louisville. This consensus of experts suggested that the best indications for laparoscopy were solitary lesions less than 5 cm, located in the anterior segments. Nonetheless, adequacy of margins is obtained keeping an adequate distance of the nodule from the line of transection; also, LLR should be far from the hepatic hilum, and the vena cava (37). However, surgical indications for LLR for HCC continued to evolve. Many authors described personal experience for LLR over the Louisville indications. Laparoscopic resection of lesions of the right hepatic lobe poses particular technical challenges (7). Yeung et al. suggests that laparoscopic anatomic monosegmentectomy of HCC located at all segments of right hepatic lobe is feasible (38). Therefore, limitation of the posterior localization of the HCC has been now overpassed. Intercostal trocars can be helpful to easily access the operative field and manipulate the instruments (39,40). However, intercostal approach may be more invasive than traditional abdominal laparoscopy.
Morioka consensus conference
The Second International Consensus Conference on LLR was held in Morioka, Japan, in 2014 to evaluate the current status of laparoscopic liver surgery and to provide strong recommendations to aid its future development (41). Moreover, tumor size limits have been overpass. HCC with a tumor size of >10 cm has been considered to be a contraindication for LLR because of concerns that the radical resection rate may be lower, and the inherent limitations of the operative procedure. However a Chinese group suggested pushing up to 10 cm of diameter the limit of HCC treatable (13). Also LLR for HCC in patients with advanced portal vein tumor thrombus has been described as a safe and feasible procedure in selected patients, when performed by surgeons with expertise in hepatic surgery and minimally invasive techniques (42).
Laparoscopic advantages and future perspectives
Concerning the morbidity, LLR generally results in improved short-term outcomes without compromising the long-term oncological outcome. In addition, the incidences of postoperative ascites and liver failure are reduced with LLR for HCC (43). Pure laparoscopic hepatectomy results in minimal postoperative ascites production, which leads to a lower risk of disturbance in water and/or electrolyte balance and hypoproteinemia. It leads to lower complications that could potentially lead to postoperative serious liver failure (44).
In very little cases some authors suggest to perform the Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) for HCC. ALPPS procedure has been described with good results with traditional access (45,46). Totally laparoscopic ALPPS is described as feasible but must be performed by experienced hands (47,48). Furthermore, performing the initial HCC resection by laparoscopy could facilitate a subsequent LT (49). It has been shown that when the initial LR is done by laparoscopy, the subsequent salvage transplantation is associated with reduced operative time, blood loss, and transfusion requirements (50,51).
Robotic approach
Since the commercialization of the da Vinci Surgical System (Intuitive Surgical, Inc., Sunnyvale, CA, USA), robotic approach is now being used for even the most complex minimally invasive surgeries. First report of robotics in liver surgery dates back to 2003 and the first series of left lateral sectionectomy to 2008 (25,52). Many study demonstrated that robotic LR is feasible and a safe procedure (30,53,54).
Advantages and disadvantages
As a minimally invasive approach, the use of robotic systems has some hypothetical advantages over traditional laparoscopy. The several limitations and drawbacks to conventional laparoscopy, including limited movement, the inability to perform high-precision sutures, unnatural positions for the surgeon and flat vision, may be overcome by robotic surgery (55). In fact the 3-dimensional view of the operative field along with 7° of freedom and tremor filtration allows the surgeon to performed delicate dissection and precise intra-corporeal suturing. Using this technology, hepatobiliary surgeon was allowed to performed resection of all liver segments and to perform complex hilar dissection, LRs requiring biliary-enteric reconstruction (56). Overall, surgical indications for robotic approach for HCC are the same of LLR. Nonetheless, the use of a robotic system can improve certain steps of minimally invasive major hepatectomy (53). Lesions located in the posterosuperior segments are with robotic system easier to perform than in laparoscopy (57). Technical limitations of LLR to achieved safe LR of posterosuperior segments overcome thanks to the ability given by the robotic system using articulated instruments and the execution of ultrasonography using dedicated robotic probes (58). Wakabayashi described robotic resection of HCC located to segment 8 with a thoracoscopic trough the diaphragm approach (59). Lai et al. recently reported two cases of robot-assisted laparoscopic partial caudate lobe resection in patients with HCC, both of them with a Child A score (60). The most convincing indications for robotic surgery are procedures that involve a small, deep, fixed operating field or when fine dissection and parenchyma sparing is required as in cirrhotic patients.
The main limitation of robotic system is the higher cost between laparoscopy. Besides, the range of instruments available for robotic liver surgery is currently much smaller than for laparoscopic or open techniques.
Prospective view
The latest innovative procedures with robot are augmented reality (28), and the single incision approach (61). As for the LLR, robotic LR for HCC has been described as a bridge to LT (27). The stable magnified field, 3-D vision, and enhanced instrument articulation facilitate the vascular and biliary dissection of the right pedicle, and this helps in deciding the point of transaction (62). We discuss about totally laparoscopic ALPPS, however, robotic ALPPS may have a place for HCC patients (63).
Conclusions
Indications for laparoscopic resection, robotic assisted and totally robotic resection of HCC will be doubtless increased in future years. LLR and robotic approach for HCC is safe and feasible. Prospective comparative study should be designed to confirm the advantages and indications of laparoscopy and robotic management of HCC.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet 2003;362:1907-17. [Crossref] [PubMed]
- Ettorre GM, Levi Sandri GB. Laparoscopic approach for hepatocellular carcinoma: where is the limit? Chin J Cancer Res 2014;26:222-3. [PubMed]
- Guerra F, Levi Sandri GB. The problem of the most appropriate curative treatment for hepatocellular carcinoma. When to embolize? When to operate? J Hepatol 2015;63:280-1. [Crossref] [PubMed]
- Ettorre GM, Laurenzi A, Lionetti R, et al. Laparoscopic liver resections in normal and cirrhotic livers: a retrospective analysis in a tertiary hepato-biliary unit. Dig Liver Dis 2014;46:353-7. [Crossref] [PubMed]
- Chen HY, Juan CC, Ker CG. Laparoscopic liver surgery for patients with hepatocellular carcinoma. Ann Surg Oncol 2008;15:800-6. [Crossref] [PubMed]
- Cho JY, Han HS, Yoon YS, et al. Feasibility of laparoscopic liver resection for tumors located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumor location. Surgery 2008;144:32-8. [Crossref] [PubMed]
- Yoon YS, Han HS, Cho JY, et al. Total laparoscopic liver resection for hepatocellular carcinoma located in all segments of the liver. Surg Endosc 2010;24:1630-7. [Crossref] [PubMed]
- Belli G, Fantini C, Belli A, et al. Laparoscopic liver resection for hepatocellular carcinoma in cirrhosis: long-term outcomes. Dig Surg 2011;28:134-40. [Crossref] [PubMed]
- Ker CG, Chen JS, Kuo KK, et al. Liver Surgery for Hepatocellular Carcinoma: Laparoscopic versus Open Approach. Int J Hepatol 2011;2011:596792.
- Yoon YS, Han HS, Cho JY, et al. Laparoscopic approach for treatment of multiple hepatocellular carcinomas. Surg Endosc 2012;26:3133-40. [Crossref] [PubMed]
- Kobayashi S, Nagano H, Marubashi S, et al. Hepatectomy based on the tumor hemodynamics for hepatocellular carcinoma: a comparison among the hybrid and pure laparoscopic procedures and open surgery. Surg Endosc 2013;27:610-7. [Crossref] [PubMed]
- Soubrane O, Goumard C, Laurent A, et al. Laparoscopic resection of hepatocellular carcinoma: a French survey in 351 patients. HPB (Oxford) 2014;16:357-65. [Crossref] [PubMed]
- Ai JH, Li JW, Chen J, et al. Feasibility and safety of laparoscopic liver resection for hepatocellular carcinoma with a tumor size of 5-10 cm. PLoS One 2013;8:e72328. [Crossref] [PubMed]
- Long TC, Bac NH, Thuan ND, et al. Laparoscopic liver resection: 5-year experience at a single center. Surg Endosc 2014;28:796-802. [Crossref] [PubMed]
- Kim SJ, Jung HK, Lee DS, et al. The comparison of oncologic and clinical outcomes of laparoscopic liver resection for hepatocellular carcinoma. Ann Surg Treat Res 2014;86:61-7. [Crossref] [PubMed]
- Yoon SY, Kim KH, Jung DH, et al. Oncological and surgical results of laparoscopic versus open liver resection for HCC less than 5 cm: case-matched analysis. Surg Endosc 2015;29:2628-34. [Crossref] [PubMed]
- Yamashita Y, Ikeda T, Kurihara T, et al. Long-term favorable surgical results of laparoscopic hepatic resection for hepatocellular carcinoma in patients with cirrhosis: a single-center experience over a 10-year period. J Am Coll Surg 2014;219:1117-23. [Crossref] [PubMed]
- Han DH, Choi SH, Park EJ, et al. Surgical outcomes after laparoscopic or robotic liver resection in hepatocellular carcinoma: a propensity-score matched analysis with conventional open liver resection. Int J Med Robot 2016;12:735-742. [PubMed]
- Shehta A, Han HS, Yoon YS, et al. Laparoscopic liver resection for hepatocellular carcinoma in cirrhotic patients: 10-year single-center experience. Surg Endosc 2016;30:638-48. [Crossref] [PubMed]
- Song J, Wang Y, Ma K, et al. Laparoscopic hepatectomy versus radiofrequency ablation for minimally invasive treatment of single, small hepatocellular carcinomas. Surg Endosc 2016;30:4249-57. [PubMed]
- Ettorre GM, Levi Sandri GB, Santoro R, et al. Laparoscopic liver resection for hepatocellular carcinoma in cirrhotic patients: single center experience of 90 cases. Hepatobiliary Surg Nutr 2015;4:320-4. [PubMed]
- Takahara T, Wakabayashi G, Nitta H, et al. Laparoscopic liver resection for hepatocellular carcinoma with cirrhosis in a single institution. Hepatobiliary Surg Nutr 2015;4:398-405. [PubMed]
- Xiang L, Xiao L, Li J, et al. Safety and feasibility of laparoscopic hepatectomy for hepatocellular carcinoma in the posterosuperior liver segments. World J Surg 2015;39:1202-9. [Crossref] [PubMed]
- Buchs NC, Volonte F, Pugin F, et al. Augmented environments for the targeting of hepatic lesions during image-guided robotic liver surgery. J Surg Res 2013;184:825-31. [Crossref] [PubMed]
- Choi SB, Park JS, Kim JK, et al. Early experiences of robotic-assisted laparoscopic liver resection Yonsei Med J 2008;49:632-8. [Crossref] [PubMed]
- Lai EC, Tang CN, Yang GP, et al. Multimodality laparoscopic liver resection for hepatic malignancy--from conventional total laparoscopic approach to robot-assisted laparoscopic approach. Int J Surg 2011;9:324-8. [Crossref] [PubMed]
- Panaro F, Piardi T, Cag M, et al. Robotic liver resection as a bridge to liver transplantation. JSLS 2011;15:86-9. [Crossref] [PubMed]
- Pessaux P, Diana M, Soler L, et al. Towards cybernetic surgery: robotic and augmented reality-assisted liver segmentectomy. Langenbecks Arch Surg 2015;400:381-5. [Crossref] [PubMed]
- Croner RS, Perrakis A, Brunner M, et al. Pioneering Robotic Liver Surgery in Germany: First Experiences with Liver Malignancies. Front Surg 2015;2:18. [Crossref] [PubMed]
- Choi GH, Choi SH, Kim SH, et al. Robotic liver resection: technique and results of 30 consecutive procedures. Surg Endosc 2012;26:2247-58. [Crossref] [PubMed]
- Lee JH, Han DH, Jang DS, et al. Robotic extrahepatic Glissonean pedicle approach for anatomic liver resection in the right liver: techniques and perioperative outcomes. Surg Endosc 2016;30:3882-8. [Crossref] [PubMed]
- Guerra F, Amore Bonapasta S, Annecchiarico M, et al. Robot-integrated intraoperative ultrasound: Initial experience with hepatic malignancies. Minim Invasive Ther Allied Technol 2015;24:345-9. [Crossref] [PubMed]
- Dagher I, Belli G, Fantini C, et al. Laparoscopic hepatectomy for hepatocellular carcinoma: a European experience. J Am Coll Surg 2010;211:16-23. [Crossref] [PubMed]
- Gaillard M, Tranchart H, Dagher I, et al. Laparoscopic liver resections for hepatocellular carcinoma: current role and limitations. World J Gastroenterol 2014;20:4892-9. [Crossref] [PubMed]
- Edwin B, Nordin A, Kazaryan AM. Laparoscopic liver surgery: new frontiers. Scand J Surg 2011;100:54-65. [PubMed]
- Nguyen KT, Gamblin TC, Geller DA. Laparoscopic liver resection for cancer. Future Oncol 2008;4:661-70. [Crossref] [PubMed]
- Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825-30. [Crossref] [PubMed]
- Yeung YP. Laparoscopic anatomic monosegmentectomy of hepatocellular carcinoma of the right hepatic lobe. Surg Laparosc Endosc Percutan Tech 2012;22:e259-62. [Crossref] [PubMed]
- Lee W, Han HS, Yoon YS, et al. Role of intercostal trocars on laparoscopic liver resection for tumors in segments 7 and 8. J Hepatobiliary Pancreat Sci 2014;21:E65-8. [Crossref] [PubMed]
- Ishizawa T, Gumbs AA, Kokudo N, et al. Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg 2012;256:959-64. [Crossref] [PubMed]
- Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 2015;261:619-29. [PubMed]
- Nakahira S, Takeda Y, Katsura Y, et al. Laparoscopic left hepatectomy with tumor thrombectomy in patients with hepatocellular carcinoma concomitant with advanced portal vein tumor thrombus. Surg Endosc 2014;28:3505. [Crossref] [PubMed]
- Morise Z, Ciria R, Cherqui D, et al. Can we expand the indications for laparoscopic liver resection? A systematic review and meta-analysis of laparoscopic liver resection for patients with hepatocellular carcinoma and chronic liver disease. J Hepatobiliary Pancreat Sci 2015;22:342-52. [Crossref] [PubMed]
- Morise Z, Kawabe N, Kawase J, et al. Pure laparoscopic hepatectomy for hepatocellular carcinoma with chronic liver disease. World J Hepatol 2013;5:487-95. [Crossref] [PubMed]
- Vennarecci G, Laurenzi A, Levi Sandri GB, et al. The ALPPS procedure for hepatocellular carcinoma. Eur J Surg Oncol 2014;40:982-8. [Crossref] [PubMed]
- Levi Sandri GB, Lai Q, Rayar M, et al. ALPPS procedure for hepatocellular carcinoma with macrovascular thrombosis: a new opportunity? J Hepatol 2015;62:241-2. [Crossref] [PubMed]
- Xiao L, Li JW, Zheng SG. Totally laparoscopic ALPPS in the treatment of cirrhotic hepatocellular carcinoma. Surg Endosc 2015;29:2800-1. [Crossref] [PubMed]
- Schelotto PB, Gondolesi G. Laparoscopy in ALPPS Procedure: When We Can Do It? Ann Surg 2015. [Epub ahead of print]. [Crossref] [PubMed]
- Levi Sandri GB, Vennarecci G, Santoro R, et al. Laparoscopic left liver lobectomy for hepatocellular carcinoma in a cirrhotic patient: a video report. Chin J Cancer Res 2014;26:735-6. [PubMed]
- Laurent A, Tayar C, Andréoletti M, et al. Laparoscopic liver resection facilitates salvage liver transplantation for hepatocellular carcinoma. J Hepatobiliary Pancreat Surg 2009;16:310-4. [Crossref] [PubMed]
- Casaccia M, Andorno E, Santori G, et al. Laparoscopic approach for down-staging in hepatocellular carcinoma patients who are candidates for liver transplantation. Transplant Proc 2013;45:2669-71. [Crossref] [PubMed]
- Troisi RI, Patriti A, Montalti R, et al. Robot assistance in liver surgery: a real advantage over a fully laparoscopic approach? Results of a comparative bi-institutional analysis. Int J Med Robot 2013;9:160-6. [Crossref] [PubMed]
- Giulianotti PC, Sbrana F, Coratti A, et al. Totally robotic right hepatectomy: surgical technique and outcomes. Arch Surg 2011;146:844-50. [Crossref] [PubMed]
- Berber E, Akyildiz HY, Aucejo F, et al. Robotic versus laparoscopic resection of liver tumours. HPB (Oxford) 2010;12:583-6. [Crossref] [PubMed]
- Giulianotti PC, Coratti A, Angelini M, et al. Robotics in general surgery: personal experience in a large community hospital. Arch Surg 2003;138:777-84. [Crossref] [PubMed]
- Idrees K, Bartlett DL. Robotic liver surgery. Surg Clin North Am 2010;90:761-74. [Crossref] [PubMed]
- Casciola L, Patriti A, Ceccarelli G, et al. Robot-assisted parenchymal-sparing liver surgery including lesions located in the posterosuperior segments. Surg Endosc 2011;25:3815-24. [Crossref] [PubMed]
- Bonapasta SA, Bartolini I, Checcacci P, et al. Indications for liver surgery: laparoscopic or robotic approach. Updates Surg 2015;67:117-22. [Crossref] [PubMed]
- Wakabayashi G, Sasaki A, Nishizuka S, et al. Our initial experience with robotic hepato-biliary-pancreatic surgery. J Hepatobiliary Pancreat Sci 2011;18:481-7. [Crossref] [PubMed]
- Lai EC, Tang CN. Robot-assisted laparoscopic partial caudate lobe resection for hepatocellular carcinoma in cirrhotic liver. Surg Laparosc Endosc Percutan Tech 2014;24:e88-91. [Crossref] [PubMed]
- Kandil E, Noureldine SI, Saggi B, et al. Robotic liver resection: initial experience with three-arm robotic and single-port robotic technique. JSLS 2013;17:56-62. [Crossref] [PubMed]
- Giulianotti PC, Tzvetanov I, Jeon H, et al. Robot-assisted right lobe donor hepatectomy. Transpl Int 2012;25:e5-9. [Crossref] [PubMed]
- Levi Sandri GB, Guerra F. Are We Ready to Perform Fully Minimally Invasive ALPPS? Ann Surg 2015. [Epub ahead of print]. [Crossref] [PubMed]


